The Outcomes Research Consortium is likely the most productive anesthesia research group, and includes 190 active investigators across 25 countries. The non-profit Consortium celebrates its 30th anniversary in 2020 and continues to produce top-quality perioperative research from large trials and big data analyses. The Consortium publishes a full paper or editorial every three days, for a total of over 1,500 full papers, or roughly 5% of all the high-profile clinical anesthesiology research. These papers spread across multiple journals and include top-tier publications such as the LANCET, NEJM, Anesthesiology, JAMA, the British Journal of Anaesthesia (BJA), and others.
I had the privilege of working with some of those outstanding researchers at their headquarters at the Cleveland Clinic in Ohio. For decades, the Consortium has had a private meeting during the American Society of Anesthesiologists (ASA) annual meeting. Starting in 2019, the Consortium session was made public, attracting more than 250 people during its initial session.
Below is the summary of the major results presented at the meeting which was led by Dr. Daniel I. Sessler, the Michael Cudahy Professor & Chair of the Department of Outcomes Research at the Cleveland Clinic.
Anemia and 'MINS'
Myocardial injury after non-cardiac surgery (MINS) is common in adult patients with an incidence of about 8% of all procedures. There are thus about 10 million postoperative myocardial ischemic events per year, each having about a 10% 30-day mortality. The mechanism is multi-factorial, but supply-demand mismatch probably predominates. Anemia is also a common finding in hospitalized patients and causes supply-demand mismatch especially when combined with stress from a surgical procedure. There have been no major published trials evaluating the influence of perioperative anemia on MINS. The authors therefore conducted two large registry analyses to evaluate the potential relationship.
The first analysis included patients presenting for non-cardiac surgery at the Cleveland Clinic (Ohio, USA) who were at least 45 years of age and had at least one postoperative fourth generation troponin T measurement documented. Nearly 4,500 patients were analyzed and the incidence of MINS was 3.5%, which correlated inversely with hemoglobin level. The second analysis included more than 7,000 patients from the POISE-2 trial in whom adjudicated myocardial infarction (MI) and/or death was the primary outcome. In that analysis, a 1g/dl reduction in hemoglobin was associated with a 50% increased risk of MI, mostly seen at hemoglobin levels below 11g/dl. These results are important for two reasons. The first is the recognition that relatively small reductions in hemoglobin are associated with large increases in the incidence of MI or myocardial injury which are potentially fatal events. And the second is that hemoglobin is a modifiable risk factor and thus potentially amenable to treatment. The two analyses will soon be published in the BJA.
Assisted Fluid Management Software Guidance for Intraoperative Fluid Administration
Individualized fluid therapy, namely goal-directed fluid management, has been recommended by various groups but is not routinely used in most centers. One reason may be that the systems are relatively difficult to use. With the primary goal of optimizing stroke volume (SV) increase, the investigators tested an automated protocol to recommend intraoperative fluid boluses and measure the effect of these boluses hemodynamically. The tested software accepts user input in the form of required/expected SV increase, real-time blood pressure monitoring from an arterial transducer, as well as fluid bolus details. The built-in algorithm assesses the need for a fluid bolus based on population prediction models and measures the effect of an administered fluid bolus on hemodynamics. A software-recommended fluid bolus can be accepted or declined by the clinician, who may also elect to administer a bolus at any time during the procedure. The investigators aimed to quantify how often fluid boluses achieved appropriate increases in SV when prompted by the software or administered by the clinician otherwise. The study involved nine U.S. hospitals and enrolled 330 adults. Whenever a clinician decided to administer a bolus, the SV increased by 8% as opposed to a 16% increase when a bolus was given after a software recommendation. The a priori set target SV increase occurred in 40% of clinician administered boluses and 60% of the software-recommended boluses. These results indicate the software integration resulted in a more efficient SV increase, which occurred more frequently than when a bolus was initiated by the clinician. A large trial is required to evaluate outcome benefits.
Supplemental Intraoperative Oxygen and Long-term Mortality
Supplemental oxygen was proposed as a way to reduce surgical site infections. Although initial trials were positive, more recent ones, including the largest by far, showed no benefit. One trial, PROXI, enrolled 1,400 patients and concluded that supplemental oxygen increases mortality, especially in cancer patients. In a secondary analysis of a cross-over cluster trial, the investigators evaluated long-term mortality in about 5,000 patients. There was no difference in mortality in patients assigned to 30% or 80% intraoperative inspired oxygen in the entire group, or in those with cancer. There is currently no convincing clinical evidence that supplemental oxygen up to 80% is harmful.
Effect of Epidural-General Anesthesia on Perioperative and Long-term Outcomes After Non-Cardiac Surgery
Observational studies suggest that epidural anesthesia may reduce postoperative delirium, however, published literature is limited and inconsistent. This five-center study enrolled more than 1,700 patients over 60 years of age to detect the effect of combining patient-controlled epidural analgesia with general anesthesia on the incidence of postoperative delirium and cancer recurrence after major surgery. Each of these outcomes is important in its own right: post-operative delirium occurs commonly and is associated with worse outcomes, and cancer recurrence is a major cause of cancer death. The hypothesis was that decreasing pain may prevent the occurrence of delirium, and that decreasing the surgical stress as well as avoiding volatile anesthetics and opioids may avoid the immunosuppressive effects observed post-operatively. At seven days post-operatively, the epidural analgesia group displayed significantly less delirium (hazard ratio 0.35, a factor of three reduction). Interestingly, this group also displayed less intraoperative hypertension at the cost of more hypotension and need for vasopressors. Post-operative pain and opioid consumption were understandably also reduced in the epidural group. The two groups did not differ in the incidence of cancer recurrence over the eight-year follow up period after adjustment for predefined factors. The result is important as this is the first large trial on major surgery showing that regional anesthesia does not reduce the risk of cancer recurrence after multiple reports claiming it might. It also shows that epidural anesthesia reduces post-operative delirium despite causing hypotension, a factor that had been postulated to cause delirium.
Epidural Anesthesia-Analgesia and Recurrence-Free Survival After Lung Cancer Surgery
Death following lung cancer surgery is largely due to cancer recurrence. Observational studies suggest that epidural anesthesia might help preserve host defenses by reducing the exposure to general anesthetics and opioids, blocking pain pathways, and attenuating inflammation and the surgical stress response. This study enrolled a total of 400 patients with non-small cell lung cancer presenting for potentially curative resection. Patients were randomized to general anesthesia with or without epidural analgesia. As would be expected, the epidural analgesia group required less post-operative opioid, but more importantly were less likely to require ICU admission, discharged earlier from the hospital, and had less pain. There were no statistically significant or clinically meaningful differences in recurrence-free survival up to 50 months. This trial convincingly shows that regional analgesia does not reduce cancer recurrence. This trial joins the one reported just above and a previously published 2,100 patient trial of paravertebral blocks for breast cancer (Sessler, Lancet 2019). There have now been about 3,500 cancer patients randomized to combined regional and general anesthesia versus general anesthesia alone with compelling evidence that regional analgesia is not protective for cancer recurrence. Regional analgesia has many benefits, but reducing cancer recurrence does not appear to be among them.
Prolonged Blood Storage Doesn't Increase the Risk of Transfusion-Related AKI
AKI is a common ailment affecting 7–18% of hospitalized patients annually and leads to worse outcomes including stroke, cardiac events, increased hospital length of stay, and mortality. Red blood cells are stored for up to 42 days according to blood bank policies and prolonged storage has been shown to induce physiological changes such as a decrease in pH, decreased 2,3-Bisphosphoglyceric acid causing reduced oxygen availability to tissues, increased red cell lysis with concomitant increases in lactate, potassium, and free hemoglobin, decreased overall viability of red cells, and increased metabolic waste products. This study is a sub-analysis of the INFORM trial in which about 25,000 patients were randomized to older or fresher bank blood. The primary result was comparable in-hospital mortality. The current analysis includes more than 8,000 patients who were similar at baseline on age, gender, ABO type, baseline creatinine, and baseline hemoglobin. There was no statistically significant or clinically meaningful difference in the incidence of AKI between the groups. Therefore, prolonged blood storage, per se, does not increase the risk of AKI and, by extension, current blood bank strategies of releasing the older units first remains justified. Importantly, all patients in this trial were transfused. The results do not mean that blood transfusions are benign; they are still a “liquid transplant” with risks and complications.
Anesthetic Depth and Delirium after Major Surgery
The causes of post-operative delirium remain unclear, but “deep” anesthesia may contribute. The BALANCED trial studied the influence of depth of anesthesia (bispectral index of 35 versus 50) on mortality in more than 6,000 randomized patients and concluded that there was no statistically significant effect. The current sub-study evaluated about 500 BALANCED patients who had delirium and long-term cognitive function assessments. Delirium was reduced by a third in patients randomized to light anesthesia, and those patients were only 1/3 as likely to suffer cognitive decline one year after surgery. Avoiding deep anesthesia is the first convincing treatment for postoperative delirium and cognitive dysfunction, both of which remain critical important patient-oriented problems.
Dr. Saasouh completed an anesthesiology residency at the American University of Beirut (Lebanon), a research fellowship at the Cleveland Clinic Department of Outcomes Research (Ohio) where he was chief research fellow, received training in Neuroanesthesiology at the Cleveland Clinic (Ohio), and is currently an anesthesiology resident at the Detroit Medical Center (Michigan). Dr. Saasouh was a 2019 –2020 Doximity Conference Fellow. He took part in the Outcomes Research Consortium discussed in this article.
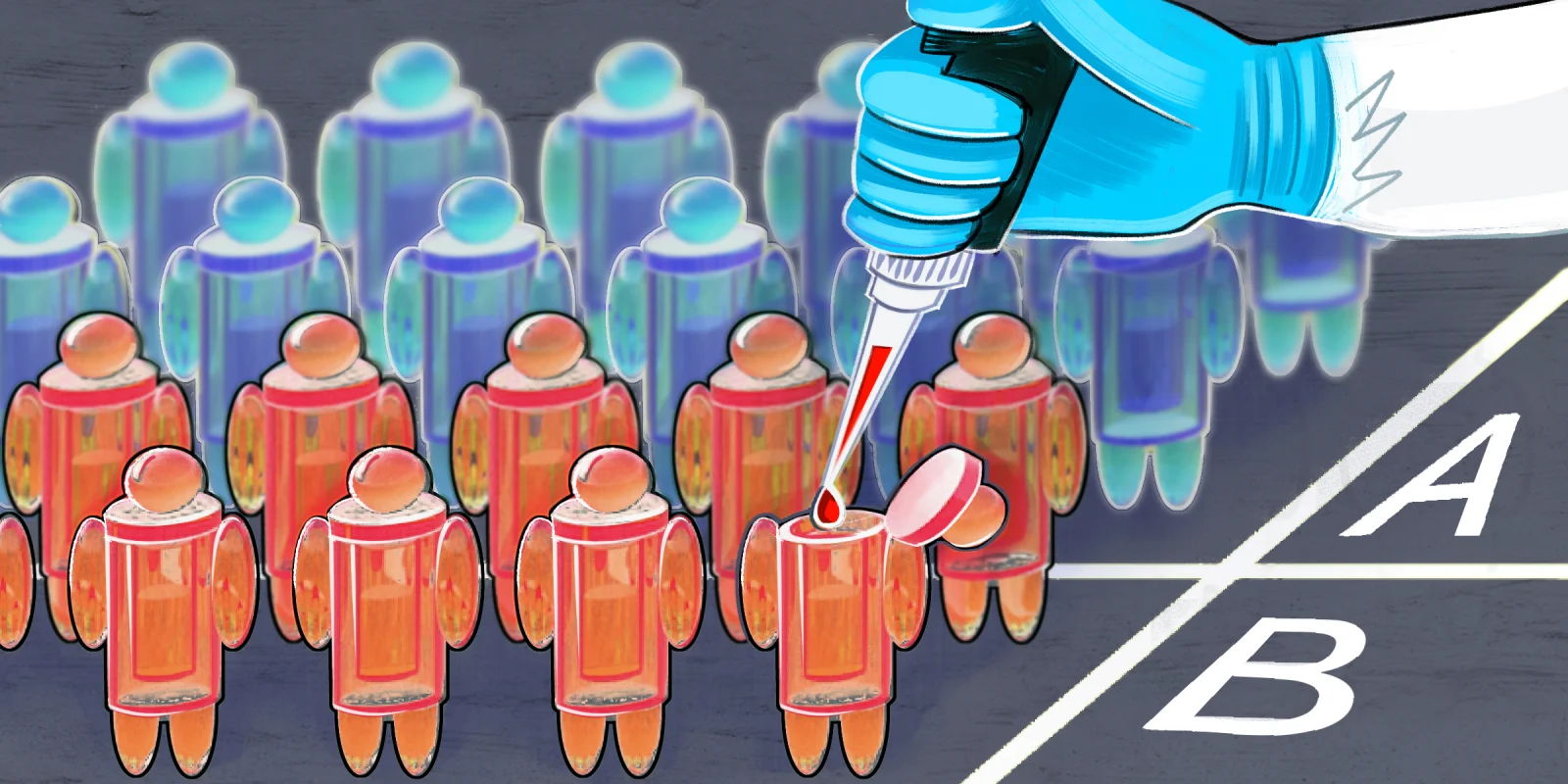
Illustration by April Brust