The 2020 American Society of Transplantation and Cellular Therapy meeting in Orlando showcased the scientific advances in the field of hematopoietic cell transplantation and CAR-T/immune effector cell (IEC) therapies. What was different and commendable about this meeting was that the enthusiasm about the innovative advances was very rightly tempered with concerns about affordability and sustainability of some of these high price tag treatments (such as $475,000 for tisagenlecleucel and $373,000 for axicabtagene ciloleucel, along with costs associated with care and management of complications).
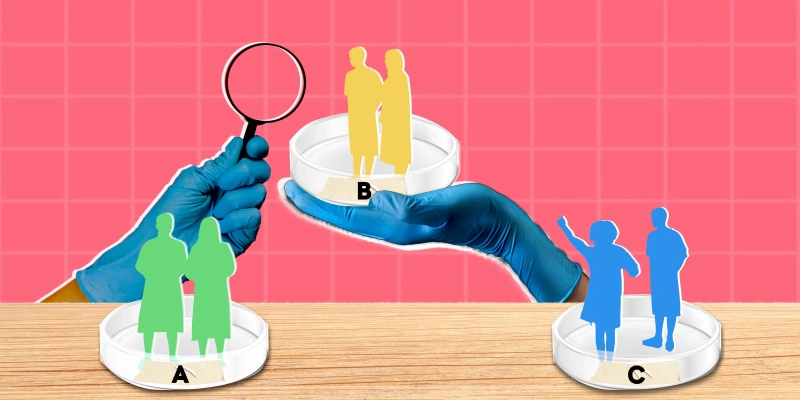
Speakers at various sessions addressing these concerns ranged from health policy experts, physician and payer leaders, to patient advocates. While a minority of the audience at these sessions felt that the concerns about the economics of these treatments may be "much ado about nothing," a majority agreed that we need to brace ourselves for a "sea change" as result of these treatments. Perspectives of different stakeholders were openly discussed, as were the knowledge gaps, policy challenges, access, and reimbursement issues around these therapies. Because of the high costs and availability in only selected centers, concern was raised about "access deserts" for these treatments.
Fred LeMaistre MD, Senior Vice President, Market Operations at Sarah Cannon, provided an example of an elderly patient with diffuse large B cell lymphoma living in El Paso needing CAR-T cell treatment that was helpful in highlighting the patient- and provider-level barriers. These multi-level challenges were proposed to be the reason by Stephanie Farnia, MPH, Director, Gene Therapy and Cellular Immunotherapy at Blue Cross Shield, as to why these treatments have been utilized to only less than 20% of their potential in the two years of their being approved commercially. Concerns about these therapies with high cost but uncertain value were framed nicely in a broader discussion of issues around waste in health care, value of new therapies, and the current and possibly future political landscape, which will affect health care economics and policy.
The need for quality measures around these newer treatments was highlighted to ensure that all six domains of quality framework — safety, effectiveness, timeliness, efficiency, patient centeredness, and equity — are met when trying to implement these therapies on a large scale. It is clear that quality shouldn’t be compromised to improve access as these are highly complicated and resource intensive treatments. Implementing these therapies in non-FACT (Foundation for the Accreditation of Cellular Therapy) accredited centers may broaden the access but could backfire due to lack of minimum guidelines for programs, facilities, and individuals performing cellular therapy .Longer term data and better identification of patient characteristics to predict the group of patients that will benefit the most is eagerly awaited. A number of proposals examining the issues around access and health care utilization of CAR-T cell therapies were discussed at the newly formed Cellular Immunity working committee of the Center for International Blood and Marrow Transplant Research (CIBMTR). Valuable clinical and sociodemographic data on patients receiving these therapies is being collected by CIBMTR through its registry function and will form the basis of studies around the issues of access and resource utilization of these treatments.
There is no doubt that access issues are more problematic for Medicare/ Medicaid beneficiaries because of the huge gap between the actual cost and reimbursement from Centers for Medicare and Medicaid Services (CMS) for these treatments. According to Dr. Farnia's presentation at TCT, even with an increase in the New Technology Add-on Payment (NTAP) from 50% to 65% for using these treatments in Medicare beneficiaries, the inadequate reimbursement is a nightmare for patients as well as providers. It remains to be seen if the changes in the payment landscape, such as renewal of the NTAP associated with payments or creation of a new DRG, will lessen the gap. Recommendations from MIT FoCUS (Financing and Reimbursement of Cures in the U.S.) project that has brought all the relevant stakeholders around the table to develop some of these novel solutions were discussed. Value-based purchasing to align payment with value of the treatment and to ensure that stakeholders have skin in the game was proposed as one solution to the problem. The need for novel payment models to help facilitate the access and utilization of these potentially curative therapies with large upfront costs and downstream benefits was emphasized. Innovation in science can only be useful if it occurs along with flexible and nimble reimbursement policies. This is currently lacking as Medicare takes a long time to change from their traditional policies.
A lot of questions, though implied, were not discussed in open. Will these million dollar treatments widen the chasm between the "haves and the have nots"? Does it really benefit a patient to treat them with a million dollar treatment just to have them go home to an empty refrigerator because they are not able to afford the basic necessities of life? Are we headed to an era where a small group of patients, based on their ability to pay, will be able to receive the "state of the science" treatment and a majority won't be able to even afford insulin or an EpiPen? How is the Medicare trust fund going to stay healthy when the number of beneficiaries, as well as the payments coming out of it, are outpacing what is going in it? With the exploding list of new sophisticated diagnostics and therapeutics, when would we concede that we are out of options to treat cancer? These are difficult questions that will be faced by patients, providers, policy makers, and payers in days to come.
We are immensely grateful for the research that has changed the way we treat cancer leading to improved cancer-specific survival across the board. As more of these products in the pipeline emerge — not only for hematological malignancies but also solid tumors — the number of patients who will be candidates for these treatments will rise exponentially. It does appear that our practice of spending millions of dollars on developing innovative medical therapies but ignoring the research around optimal health care delivery for these therapies has led to this "tsunami" for which our society is not prepared. But, maybe we can still salvage the situation as we prepare for an onslaught of these high-cost complicated treatments. This meeting certainly reflected on the efforts indicating the fact that we are not burying our head in the sand but taking this challenge head-on!