About five years ago, I remember sitting in morning rounds during my third-year inpatient psychiatry rotation. I heard them mention a new patient, an older woman with a traditionally Punjabi last name, which caught my attention.
“She wears a headscarf and doesn’t speak any English. Good luck.” Everyone chuckled, some rolled their eyes.
Suddenly, I felt my throat tighten and my muscles tense. I had never met this patient, but I felt a mixture of fury and concern for her not only as a medical student but also as a Punjabi woman. I held in the barrage of questions that popped into my mind, distilling them down to one for the attending I was working with after rounds: Can I help take care of her?
The patient wore a salwar kameez and head covering, like the nurse had mentioned. I observed how her shoulders were hunched, her gaze was determinedly directed down, and her arms were crossed. Walking over, I said hello — Sat Sri Akal — in Punjabi. Softly, she asked if I could speak Punjabi; I told her that I could speak some, though I was not fluent, and noticed how despite this her posture slowly started to become more open.
Over the next week, in bits and pieces this patient began to trust our team with her history and her experiences. She shared the depth of her intense isolation in this country, the generational divides between her and her children, and the difficulty she sometimes had putting words to her feelings, even in Punjabi. Each day, as I left the unit, she begged me not to go. “They don’t understand me. They keep giving me things without explaining what they are.”
While we generally requested interpreters (either in person on the unit or via telephone) for our daily interviews, I realized that interpreters were not being requested for other, smaller interactions. As a result, I started to get random requests throughout the day from staff to help with this patient. Once, when she declined to take a medication, I was called to the nursing station. “It’s just a multivitamin, can you just explain that to her? I don’t have time to pull up the interpreter just for a multivitamin.”
Hearing this, I wondered what would happen if I wasn’t around. Would the staff just document this patient’s refusal and move on? What if it wasn’t just a multivitamin, but one of her medications for mood or blood pressure? Also, would anyone be willing to take a random pill without knowing what it was? When I tried to express these concerns to my team, I was instead dismissed and told how helpful it was to have me working with her.
To this day, I remain deeply unsettled by this experience. Every patient has a right to understand their medical care and treatment options. While it is important and extremely powerful to have clinicians who share a cultural background (or even a language), that should not determine the standard of care that a patient receives. It was unacceptable that when I was not around, this patient’s care suffered, and that I was managing the expectation that I would be able to “handle it” any time she expressed a need or asked a question. Furthermore, I was not certified as a professional interpreter, and assumed incorrectly that it would be better to translate as best I could rather than to burden the staff with waiting to request an interpreter.
Looking back, I wish I had been able to articulate the need for an interpreter better, though I struggled to do so as an early clerkship student working within the hierarchies of medical training. I did not know this at the time, but patients have a right to interpreter services that is mandated by federal law. As a resident, I now ensure that even if I know the language, I make the time to request a certified, professional interpreter to ensure proper care for my patients. Several studies have shown that utilizing an interpreter — specifically in person — is associated with more satisfaction and improved communication.
We know that patients with language barriers are particularly vulnerable populations in hospital settings. One study showed an increased risk of adverse events for patients with limited English proficiency (LEP). Other research has shown higher rates of medication non-adherence, poorer outcomes, and decreased comprehension of health information. One study focused on psychiatric patients in Switzerland showed that patients with lower language proficiency had higher rates of compulsory admission, compulsory medications, and seclusion/restraints. We know that staff face barriers in using tools to screen for delirium in patients with LEP, such as the Confusion Assessment Method. Anecdotally, I have seen how behavioral codes look different for patients who don’t speak English, and when getting an interpreter is not at the forefront of the list of priorities.
Ensuring our patients understand the medications we give, the procedures we perform, and the plan for their care is just the bare minimum. Language is so much more than a medium of communication. It carries history, culture, and nuance. For example, I once had a patient on an inpatient psychiatric unit who had been signed out as “hyper-religious” in the context of a manic episode. When I included an in-person interpreter in our next conversation, the interpreter was able to provide some context to the patient’s prayers that the patient could not provide herself — that it was a holiday in the patient’s home country, and that part of the tradition was to repeat her prayers on behalf of her family that wasn’t there with her to celebrate. Though the patient was still exhibiting signs of mania, this clarification allowed me to add nuance to my clinical formulation and helped me be a more empathetic physician.
Slowly, we are starting to refine medical practice as we learn about the variety in human expression and experience across cultures. Over time, we’ve moved away from the phrase ‘cultural competence’ to ‘cultural humility,’ which better encapsulates and acknowledges the complexity of identity and the curiosity with which we should approach our patients. Ensuring translation services are available for every interaction is an excellent way to start practicing the humility we preach.
How do you practice cultural humility with your own patients? Share in the comments!
Dr. Avneet Soin is a psychiatry resident in New York City. She is interested in consultation liaison psychiatry and advocacy work, and in her free time enjoys reading and exploring the dessert scene in NYC! Dr. Soin is a 2023–2024 Doximity Op-Med Fellow.
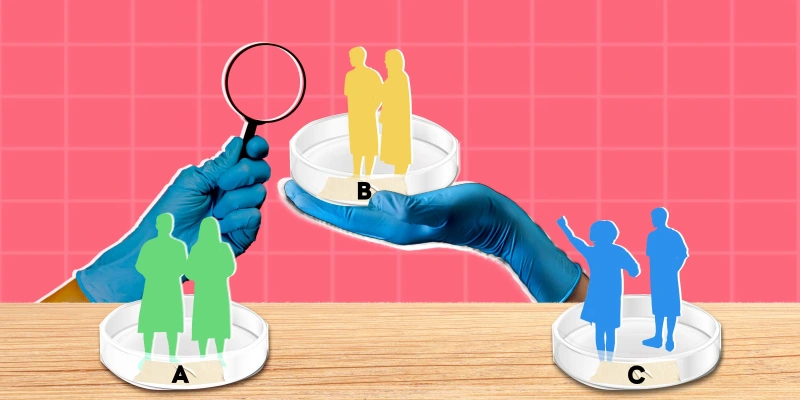
Illustration by Diana Connolly