Dr. Zhen Gooi is a 2020–2021 Doximity Research Review Fellow. Nothing in this article is intended nor implied to constitute professional medical advice or endorsement. The views expressed in this article are those of the author and do not necessarily reflect the views/position of Doximity.
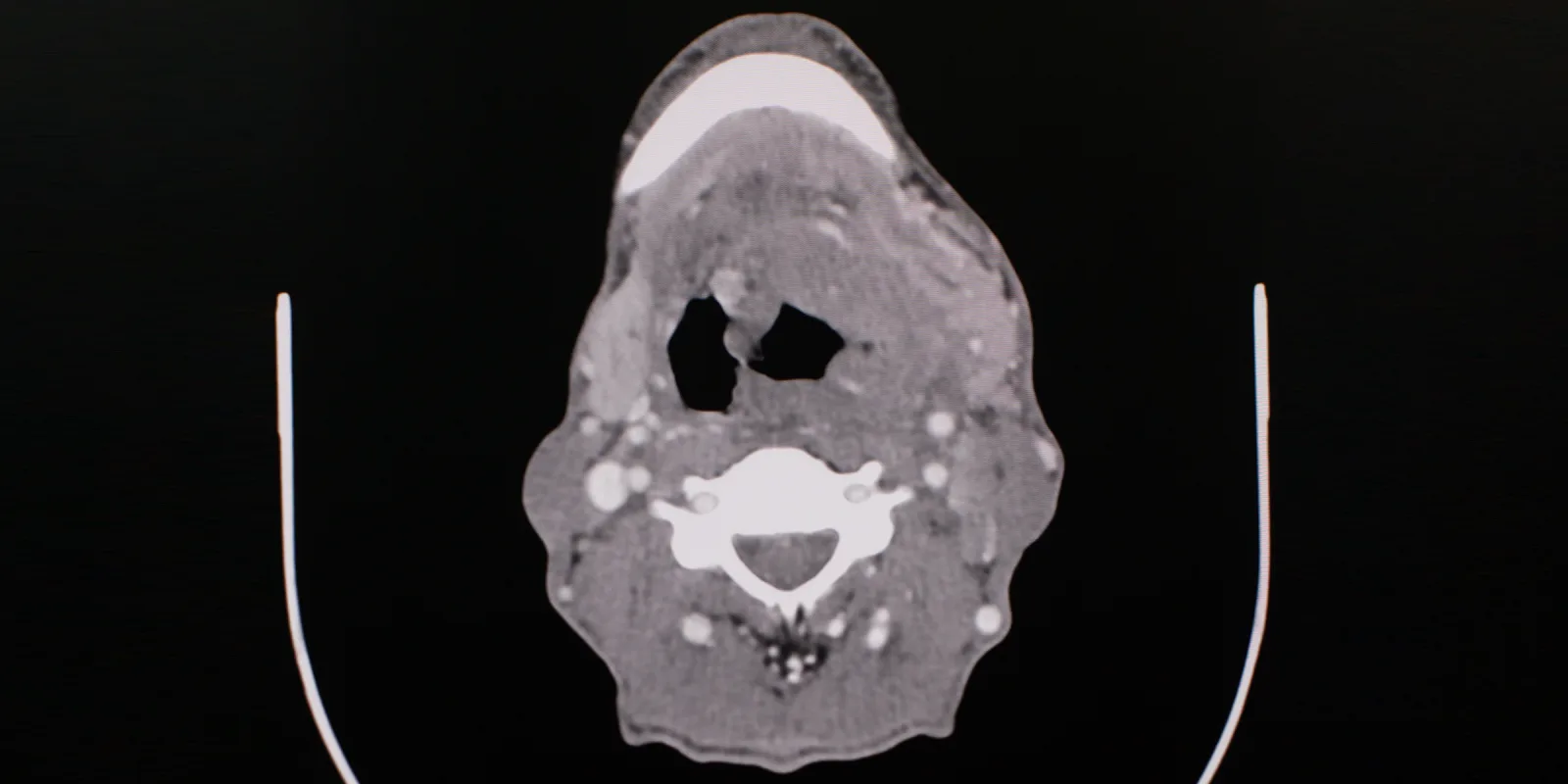
The current standard of care for locoregionally advanced HPV-associated oropharyngeal cancer involves radiation treatment to 70 Gy plus cisplatin. It has been known for some time that HPV-associated oropharyngeal cancers have better prognoses, and multiple strategies are being investigated to reduce treatment side effects associated with radiation therapy and chemotherapy.
Recently, a clinical trial by Som et. al investigated whether omission of either chemotherapy or dose reduction in radiation treatment would result in equivalent survival outcomes. The trial included patients with T1–T2, N1–N2BM0 or T3N0–N2bM0 HPV-associated oropharyngeal cancer with a less than 10-pack per year smoking history. These patients were randomized to either 60 Gy intensity modulated radiation therapy (IMRT) over a period of six weeks with weekly cisplatin (IMRT + C), or 60 Gy IMRT alone. The primary outcome of interest was 2-year progression-free survival, defined as local, regional, or distant progression or death from any cause. The MD Anderson Dysphagia Inventory (MDADI) was used to assess swallowing-related quality of life measures.
The results showed that patients in the IMRT + C arm had a 90.5% 2-year progression-free survival rate. Patients in the IMRT alone arm had a rate of 87.3%, though the difference in rates was not statistically significant. The 1-year MDADI scores did not differ significantly between groups. Grade 3–4 acute toxicities were almost 30% more common in the IMRT + C arm as compared to the IMRT alone arm, though again, the difference in incidence of late toxicities was not statistically significant.
Interestingly, the study did show a differing pattern of failure between the two treatment groups. In patients receiving IMRT + C, most failures were distant metastasis (35%); in the IMRT only arm, locoregional failure dominated (42%). The difference in locoregional failure was statistically significant between both groups. It is unclear if patients experiencing locoregional failure received successful salvage treatment.
Overall, this trial increases the body of evidence on the feasibility of radiation dose reduction for locoregionally advanced HPV-associated oropharynx cancer in patients without an extensive smoking history.
Dr. Zhen Gooi is a head and neck oncologic surgeon in academic practice at the University of Chicago. He completed his residency and fellowship training at Johns Hopkins University.
Image: Karan Bunjean / shutterstock