Telehealth helps 68% of clinicians build or maintain trust with patients who have been historically marginalized or made vulnerable, according to a recent poll on the Doximity network.
Building trust with patients has long been a critical aspect of clinical care. Yet uncertainties surrounding the COVID-19 pandemic, along with continually changing safety protocols, have in many ways unsettled the traditional patient-clinician landscape. With rapidly rising usage since the start of the pandemic, telehealth has introduced a new, digital element into the evolving dynamics of the patient-clinician relationship.
“COVID-19 has accelerated the public and professional experience of the role of technology in the health care system of the future,” wrote Drs. Bimal Shah and Kevin Schulman in a NEJM commentary. “The health care market has the opportunity to embrace the challenge to make health care better and not squander the opportunity that the pandemic has provided.”
Growing Pains
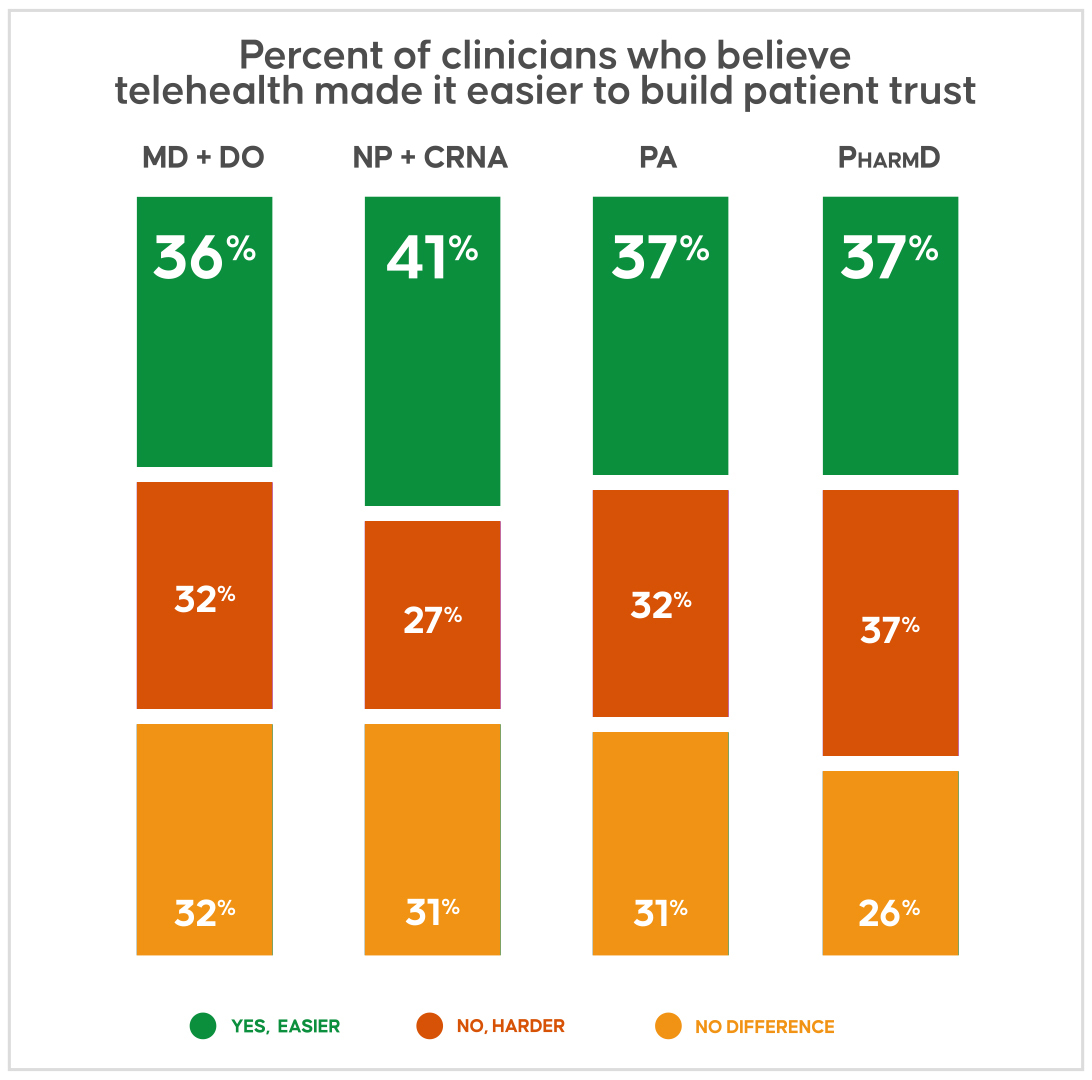
Among more than 1,600 physicians, advanced practice practitioners, and pharmacists who responded to the Doximity poll, 37% find telehealth makes it easier for them to build trust with patients who have been historically marginalized. The percentage remains similar even when categorized by different professions.
A notable percentage of clinicians at 31%, however, find telehealth makes it harder to build patient trust. And 32% believe telehealth is comparable to in-person visits in terms of building trust.
The nearly even split may reflect the growing pains of an emerging technology that has proved invaluable for certain aspects of care — all while presenting unique challenges.
In the case of historically marginalized communities in particular, telehealth has highlighted ongoing inequities in access to medical care. Research has also shown that patients who are older, identify as Black, Latinx, or Native American, and have limited English proficiency are, for myriad reasons, less likely to complete a telemedicine visit.
“We need to be really careful that telemedicine doesn’t worsen health disparities,” said Dr. Julia Frydman, an internist at Icahn School of Medicine at Mount Sinai and lead author of a study on telemedicine uptake during the pandemic.
Still, there remains broad support and optimism for the technology in the medical community, and many clinicians are opposed to rollbacks in services and reimbursement that could potentially leave vulnerable patients without care for extended periods of time. Clinicians have pointed out additional benefits of telehealth beyond better access, including increased time with patients, greater care partner engagement, and insight into a patient’s home environment, among others.
Part of the Solution
The poll results indicate that telehealth may help certain groups of clinicians build patient trust more readily than others.
Approximately 40% of clinicians in urban areas believe the technology makes it easier to build trust, compared with only 34% in rural settings. Greater familiarity and access to technology and broadband internet in urban versus rural settings may contribute to this trend. Though rising ownership and use of mobile technology among rural adults may help narrow the gap over time.
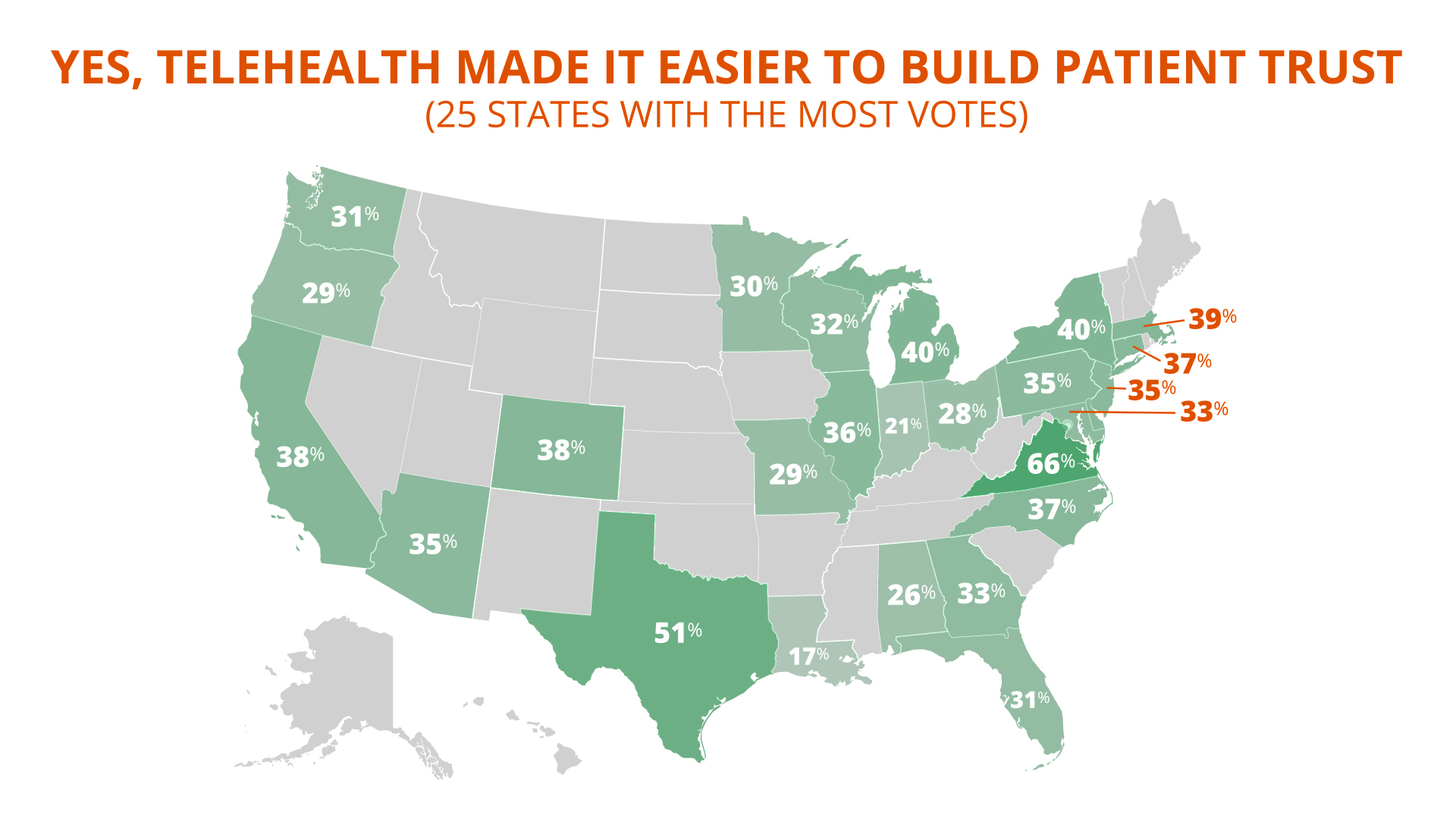
Across the U.S., roughly one third of clinicians agree that telehealth helps with trust — with notable outliers in the states of Louisiana (17%) and Virginia (66%).
Women find telehealth facilitates trust-building more often than do men. At least 40% of women say telehealth helps with patient trust, whereas only 32% of men do. The finding affirms prior reports from various telehealth platforms that both women physicians and patients favor telehealth more so than men.
Age is also a factor: 40% of clinicians in their 40s say telehealth makes trust-building easier, versus 37% for those in their 30s or 50s, and 31% for those 70 years or older. Comfort and familiarity with the technology may again be driving the trend. Studies have shown that preference for telemedicine is greater not only among clinicians who are in their 40s or younger, but for patients in the same age range as well.
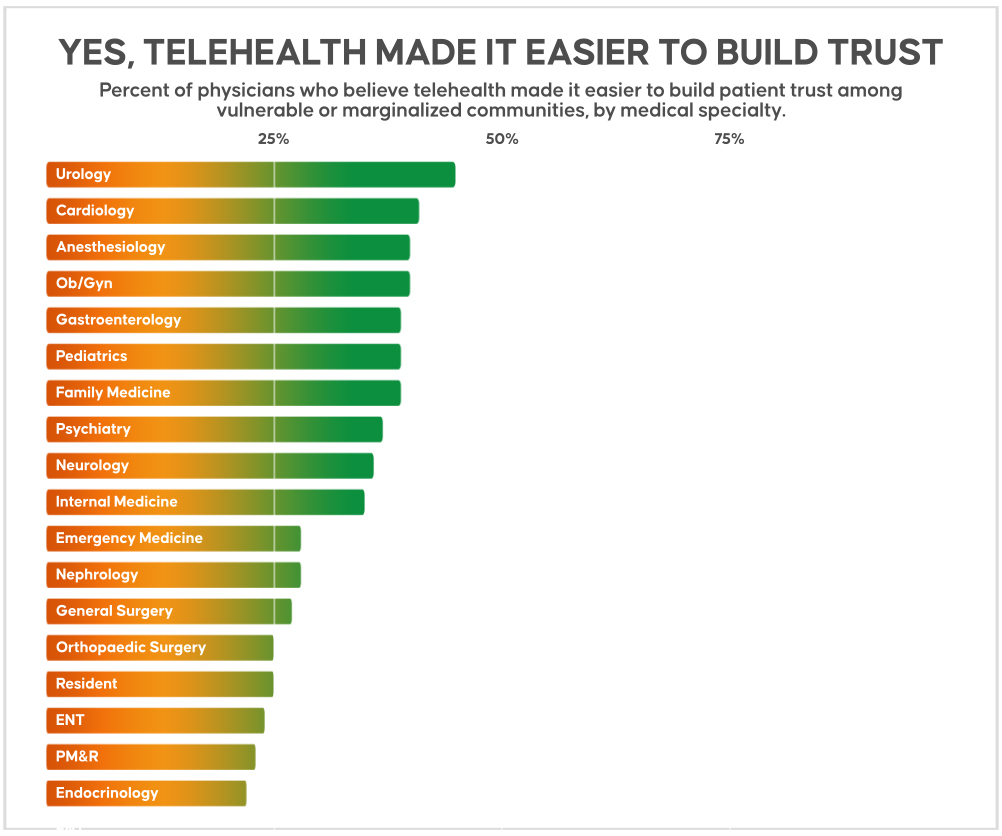
For MDs and DOs, a greater percentage of primary care physicians agree telehealth makes it easier to build trust (38%) than surgeons (30%), despite the high ranking of urology and ob/gyn. The difference aligns with the earlier adoption of telehealth by patients with chronic illnesses who likely had more time to acclimate to the technology. However, the trend is less clear when ranking by physician specialty, with urology (45%), cardiology (41%), anesthesiology (40%), ob/gyn (40%), and gastroenterology (39%) leading the way.
Collectively, the results indicate a varied experience with telehealth use — an understandable corollary of its sudden acceleration to the forefront of health care during the pandemic.
With nearly three quarters of patients planning to rely on telemedicine moving forward, patients and clinicians may benefit from strategies that improve upon existing offerings. Features such as mobile device-based telehealth, language interpretation services, audio-only options, and visual tools can help expand accessibility and address barriers that patients face. And as the technology continues to advance, telehealth’s capacity to help clinicians foster a trusting relationship with patients, especially underserved populations, may play a key role in its widespread and lasting adoption.
“Building trust requires a human connection and genuine empathy and compassion,” said Dr. Maulik A. Patel, an internist in Georgia. “And if we can demonstrate that with our words and time, trust can be built even via video.”
Image by Viktoriia Miroshnikova / GettyImages
Visualizations by Dox Digital





