“Your undergraduate degree is in journalism? That’s an odd precursor to medicine. Are you sure you’re prepared for medical school?”
This question, in one variation or another, was asked at every one of my medical school interviews. I had come prepared.
“They may seem unrelated,” I replied, “But journalism taught me how to approach new situations, gather information from a variety of sources, synthesize it, and communicate it clearly to others using spoken and written word. It seems to me this is what physicians do all day in their practices.”
Quizzical looks from my interviewers faded after hearing this.
“Well, yes, I suppose so. I’ve never thought about it that way,” one had said.
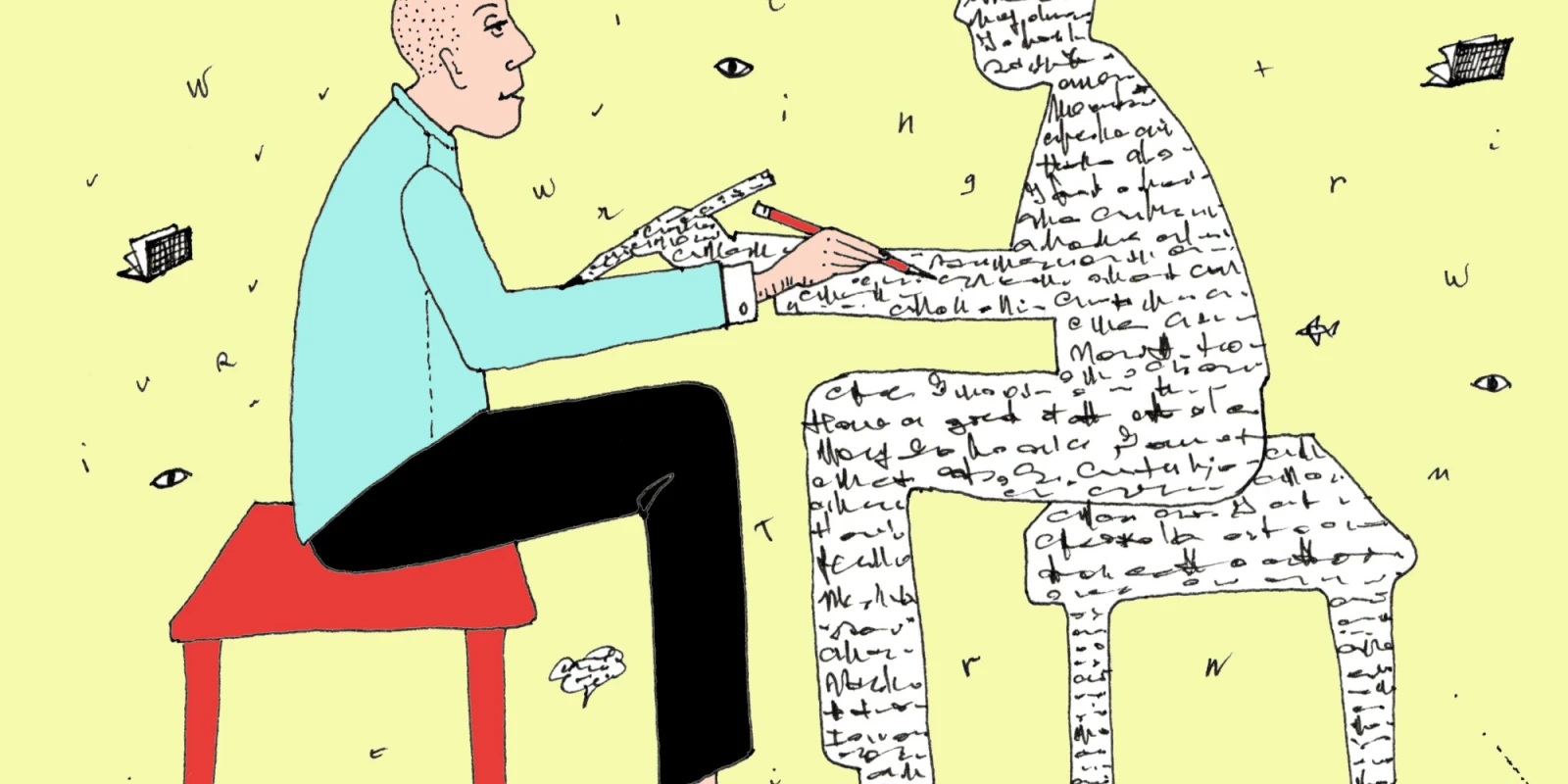
My interviews previewed what I then observed in medical school and residency. Doctors spend all day talking and writing to each other and to patients and their families. Communication is at the heart of medicine. When done well, it is a source of comfort and clarity. When done poorly, it is the source of medical error, patient dissatisfaction, and confusion.
Whether calling a consult, writing a clear discharge summary, explaining complex pathology in a way a patient can understand, or posting about health topics on social media, excellent communication is essential to our practice. Our training in such a central skill should be proportionate to its use.
However, our education in communication is often informal, implicit, and insufficient. Most medical schools provide lectures and workshops in oral presentations, as well as a few hours targeting particular types of communication such as breaking bad news or end of life conversations. Rarely are we taught explicitly how to write comprehensively yet succinctly, differentiate our style for a discharge summary, or ensure our patients truly understand the treatment plan. Much of how we learn to communicate is through observing the styles, tricks, and mistakes of those we rotate alongside on the wards. Too much is left to variable experiences of observation, poor modeling or trial and error.
Why is our formal training in written and verbal communication scant? Why was my journalism background seen as a quirk instead of an asset?
Perhaps we haven’t yet appreciated the scale of the problem. It becomes quite apparent when one trades the white coat for the gown and becomes a patient. As a cancer patient myself for the last dozen years, I’ve been told completely opposite plans by various consulting teams, read my admission notes full of mistakes, and caught medical errors stemming from inaccurate hand-offs between my day and night teams. I have watched while my family members, their brows furrowed, clearly had no understanding of the jargon my doctors used. I’ve cringed as doctors have given me bad news flippantly, awkwardly, or with a choice of words that frankly felt cruel. My life as a patient and training as a journalist have made the communication gaps in medicine glaring, showing me the unnecessary suffering poor words create. We must do better.
Forces beyond our interactions with patients and colleagues are also pushing us to communicate more expertly. The morass of copy-and-paste excessive documentation in our electronic medical records makes concise writing even more important. The trend toward “open notes” - allowing patients to read their charts online - makes the clarity of our words imperative. The proliferation of health information online, much of it false or obtuse, makes our ability to translate complex medical topics for the public more important than ever.
There are several concrete ways we can improve our communication:
- Seek medical school applicants with strong communication skills and training. Realize the skills learned from a degree in journalism, creative writing or literature translate directly to the practice of medicine. Embrace such students as assets in medicine.
- Make the teaching of written and verbal communication as comprehensive, standardized and formal as that of pathophysiology, integrating it in a scaffolded fashion at all training levels. We must learn to orient our communication to our audience, tailoring it for different situations- admission, discharge, giving results, communicating with PCPs or consultants, hand-offs, family-centered rounds, emergencies, end of life - with practice and structured feedback.
- Provide writing workshops taught by professional writers or physician-writers. Teach skills such as use of active verbs and semantic qualifiers, jargon minimization and redundancy reduction.
- Teach health literacy explicitly and experientially. Reinforce the teach-back method constantly. Recruit real patients to help teach patient-doctor communication. Routinely ask for feedback from your patients regarding your own communication.
- Integrate narrative medicine throughout training. This methodology not only hones the ability to write and reflect, but builds empathy, reduces burnout and fosters community.
- Integrate social media training. We can no longer limit our communication to the exam room. In learning to write OpEds, translate our academic writing for the lay reader, speak well in public and write engaging online content, we can extend our practice to advocate and educate outside hospital walls.
Perhaps with these measures, along with a cultural shift toward valuing communication in medicine as much as anatomy or physical exam skills, degrees like mine will no longer be seen as odd, and future patients will feel only comfort and clarity from their physicians.
Julia Bruckner, MD, MPH is a pediatrician, mother, survivor of recurrent cancer, and writer. You can find her at www.juliamd.com and @JuliaMDWriter on Twitter. She is a 2018-2019 Doximity Author.