This has been an unprecedented year in the treatment of patients with acute myeloid leukemia (AML). There have been eight new drugs introduced recently, increasing the options for therapy dramatically. The reintroduction of the anti-CD 33 antibody gentuzumab ozogamicin, the approval of a liposomal version of 3 + 7 Vyxesos, FLT 3 inhibitors midostaurin and gliteritinib, IDH 1 inhibitor ivosidenib, IDH 2 inhibitor enasidenib, sonic hedgehog inhibitor glasdegib and bcl2 inhibitor venetoclax will improve outcomes for many patients. All of these options have been developed with the cooperation between the FDA, pharmaceutical companies and academic centers to enroll patients on clinical trials to develop these drugs. In the era of molecular diagnostic tools, this has allowed for tremendous progress in a rare disease. Further progress, however, in the treatment of AML may be hampered by the lack of patients with particular molecular abnormalities to enroll in clinical trials.
One of the most important oral abstracts at ASH did not address a new treatment option but questioned whether the way we are developing drugs for rare hematologic diseases with particular molecular and immunologic characteristics can be sustained.
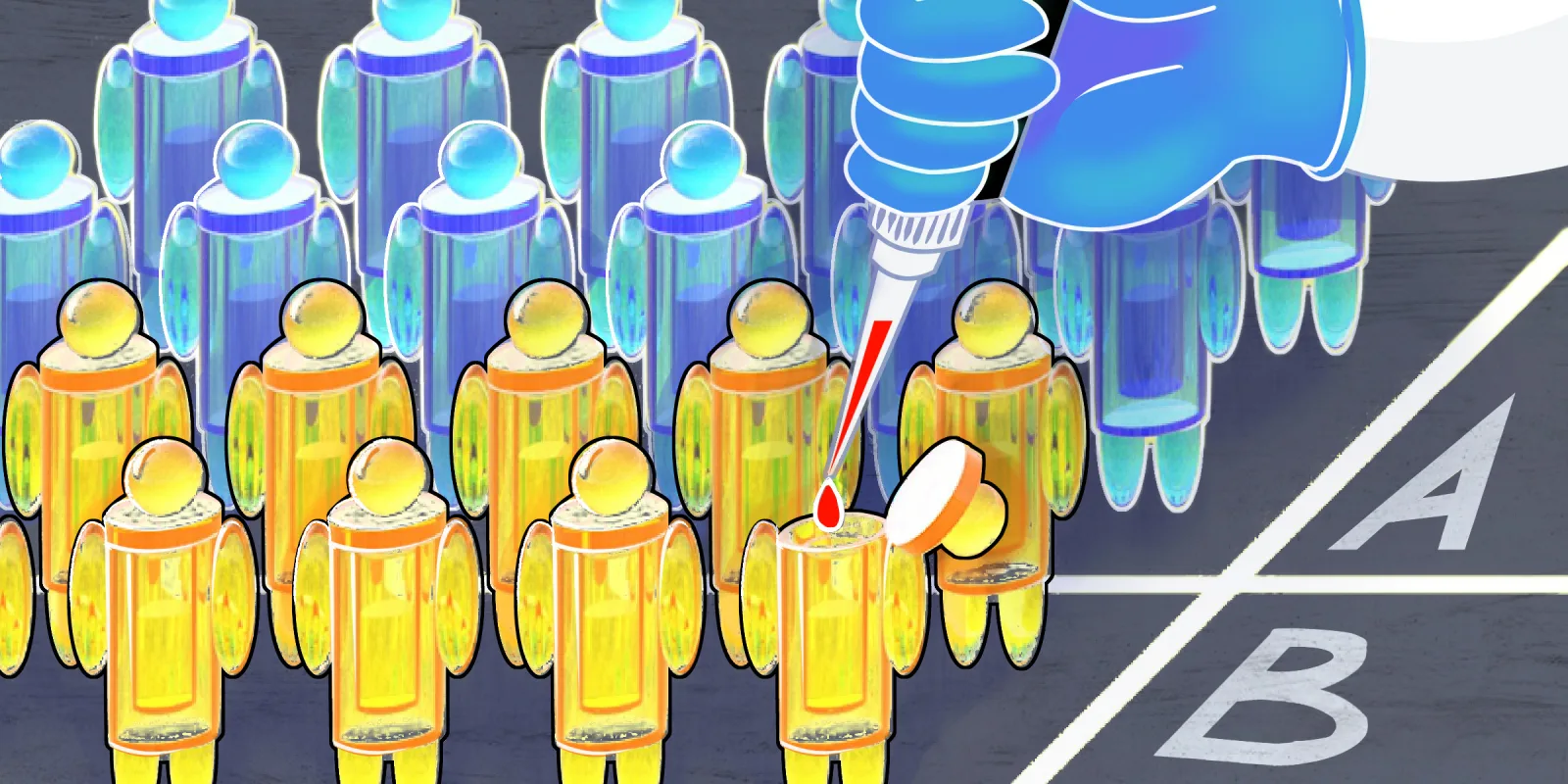
Oral abstract 713 presented by Uma Borate, MD from the Oregon Health and Science University entitled "Proportion of Patients with FLT3 Positive AML Required to Enroll on Clinical Trials to Satisfy Recruitment Needs of FLT 3 Inhibitor Trials: Are We Running Out of Patients" ponders this question. The abstract mentions that there currently are 24 FLT 3 inhibitors being investigated in clinical trials. In 2017, approximately 21,380 patients were diagnosed with AML. The rate of FLT 3 positive patients in this population is approximately 30 percent which means approximately 6,414 patients were FLT 3 positive. The rate of adult clinical trial participation in the U.S. is five percent and assuming that five percent of the FLT 3 positive patient would participate in clinical trials, approximately 320.7 FLT 3 positive patients would be expected to enroll on clinical trials. This does not satisfy the current need for FLT 3 positive patients to complete open clinical trials of FLT 3 inhibitors. In 2017, the total enrollment needed to complete these clinical trials is 1235 patients. If trials that are completed and are enrolling internationally are excluded, the total number needed in the U.S. is 844.49 patients. To complete these trials the total number of patients expected to enroll on clinical trials would need to increase to 13.2 percent which is three times the upper limit of historical normal clinical trial participation rates in the U.S.
This is sobering information. For example, IDH 2 mutations occur in just 10 percent of AML patients, and, if you do the math, just over 100 patients with an IDH 2 mutation can be expected to enroll on clinical trials in the U.S. With these numbers, it will be very difficult to finish up front trials using these drugs in combination with chemotherapy. Presumably, because other molecular mutations where targeted drugs are being developed may be even scarcer in the AML population, the progress of AML drug development given our current organizational apparatus is threatened. To remedy this problem there are going to have to be drastic changes to increase the participation of adult cancer patients on clinical trials. The question is: how to do this?
Currently there are many important barriers to clinical trial participation. Clearly, there are economic barriers. Community physicians are unwilling to send patients to academic medical centers for clinical trial enrollment because they need to maintain patients in their practice and obtain chemotherapy to keep private practice revenue stable. Insurance companies have restrictive policies on clinical trial participation and on the physicians that patients can consult for treatment. Secondly, there are too many redundant trials that do not address important questions such as which FLT 3 inhibitor is superior—midostaurin or gilteritinib—and which can be best combined with chemotherapy. This would require pharmaceutical companies to cooperate among each other to run practice-changing clinical trials.
Patients are restricted by geographic location, transportation needs, and ancillary cost of treatment at an academic facility. The apparatus has not evolved to enroll rural patients and treat them in their community or to compensate patients for transportation costs and ancillary expenses. Patients are unwilling to enroll on Phase 2 and 3 trials and be randomized to standard of care arms. Given there is historical data on patients who have received standard of care treatments, there needs to be an exploration of using this data as a control arm on treatment trials to boost patient interest and participation. Many trials have very restrictive criteria for entry that does not mirror the "real life" population of AML patients. Lastly, the disorganized and misplaced emphasis on billing in the electronic medical record has made data collection on patients participating in clinical trials difficult. The vendors of the EMR will need to partner with the FDA, pharmaceutical, and physicians to create a system where data can be collected reliably from remote sites where patients can participate in clinical trials and data can be collected without frequent trips to an academic medical center.
To address these concerns, there needs to be a re-examination of how we develop drugs for adult cancer patients in the United States. The Children's Oncology Group (COG) has been much more successful in recruiting children in cancer clinical trials with a participation rate of 50 percent. The outcomes of children with cancer are better than they are in adults in the U.S. and this might be partly because of the excellent accrual to COG trials. There needs to be cooperation between the FDA, pharmaceutical companies, organizations like ASH and ASCO, EMR vendors, academic and community physicians to find a way forward to develop drugs in the era of personalized medicine. Adult participation in cancer clinical trials must increase and the barriers to enrollment need to be addressed soon and seriously by all parties involved.
Dr. Ritchie treats myeloid malignancies including AML, MDS and MPNs and is involved in clinical trial drug administration assisting in the development of new drugs for these diseases. She works at Weill Cornell Medical College.