Community pharmacists are some of the most trusted and accessible clinicians. But when a health misadventure or unexpected illness occurs, they are the second-to-last stop on the health care train. It is the final delay between diagnosis and home. And if that stop changes from one stop to two, well, then all hell breaks loose. It doesn’t matter why there is an extra delay in care. Whether it’s from lack of insurance coverage or a drug shortage, sometimes it is the straw that breaks the camel’s back.
Increasingly, I’m finding that patients are accusing me of not caring. And it’s not just me; I’m hearing this anecdotally from friends and colleagues and seeing it posted on social media. And I can almost sympathize with the accusers. Almost. It’s true: As a community pharmacist, I cannot give every prescription as much care and attention as I used to be able to provide. I cannot individually call each office for every prior authorization. There is so much more therapy gatekeeping than there used to be. And I get it; prior authorizations are a necessary evil, if you will. We have a finite number of resources and must allocate them appropriately. I cannot call 12 other pharmacies to see if they have a backordered drug in stock. Because, one, I have multiple drugs affected by allocation and supply chain issues. And two, because sometimes it’s been in short supply for months in our area, so whatever anyone had has already been dispensed.
Now why can I almost sympathize instead of empathizing and providing more patient-centered care? It’s because of the accusation itself. The patient does not intend to call me out for personal self-improvement. Instead, they are needy and self-centered. They want me to take on more than I can handle in the current climate and focus on their problem. They are being mean and manipulative. Are they mean on purpose? Perhaps not, but still, should this behavior be rewarded? It’s not that I don’t want to help. And believe me, I do when I have time to make these phone calls. And when it’s clinically appropriate to expedite a prescription order, I can do that as well.
But in the age of e-prescribing, I have no control over how many orders are received at a time. Is there an influx of new orders at 5 p.m. on Friday? You bet, every week. And without a patient dropping off the prescription order, how am I to know that this patient hasn’t taken their lisinopril for five days, but this patient isn’t going to pick up this losartan for over a week? I can hypothesize that antibiotics will be picked up sooner rather than later. But I don’t know which clinician said go over to the pharmacy, it will be ready for you, and who is using evidence-based antimicrobial stewardship, and it’s a watchful waiting order that might never need to be picked up.
The burnout is real. It is so draining to hear that I don’t care. It feels like a personal attack. It is so exhausting when I don’t even know the last time I went home on time. I’ve stayed to do one more thing for one more patient because I promised that I would before the end of the day. The patients are the reason I show up at the pharmacy. I chose to be on the frontline, work in a public setting, and be the most accessible clinician. Being told you don’t care feels like a giant slap in the face.
I know this is not just a pharmacy problem. The whole world is worn down. How could we not be? We have endured a pandemic and have shifted our processes for everything. The medical community we depend on for care has taken a beating. The crowd has thinned because some have left the profession, fewer students have entered, and a disproportionate number of those on the front lines have died.
We chose to be medical professionals because we cared. We are clinicians. Care is in the title. And as the Dean of Students at Midwestern University Chicago College of Pharmacy once told us in a workshop, we all put on our applications that we wanted to help people. But how do we continue to help now that it’s more complicated? How do we pour from an empty cup? How, when there are complexities that make the patients depend on us even more? They need us to tell them this medication is on a national backorder, and no amount of calling or yelling on the phone will magically find it on a shelf. They need us to tell them they can use a therapeutic equivalent that is not backordered, which also may be more economical. Or maybe we have to give the bad news that they will have to wait to start their therapy. Is it fair? No. Is it the patient’s fault? No. Is it the prescriber’s fault? No. Is it the pharmacist’s fault? No. No one is at fault, but the fact remains that the patient needs a drug that the pharmacy doesn’t have.
We have to work together. We all have the same end goal to help our patients lead happy, healthy lives. We need not pit the patient against other physicians. We also need to have reasonable expectations. Writing prescriptions is more than the physical act of writing the words on paper, and filling them is more than taking pills from the big bottle and putting them in the little bottle. The practice of medicine is complex. Yes, we follow evidence and guidelines, but that does not mean that it’s cookie cutter or assembly line. Picking up a prescription through a drive-thru differs from picking up fast food. For one thing, missing a side of fries most likely will not have fatal consequences. Missing a drug interaction or an allergy very well could.
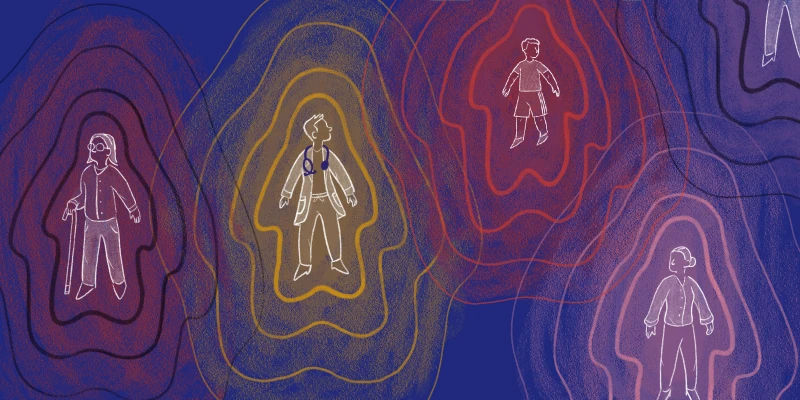
Ultimately, our patients are just trying to get the care they need. They are depending on us to treat them. Our hands are often tied in the care we can provide, but that never means we don’t care. Any outburst should not be taken as a personal attack, even though sometimes it is directed that way. Showing a little empathy can go a long way. We are human; our patients are human. Both sides need to remember that when evaluating the level of care in health care.
Has a patient accused you of not caring? Share in the comments.
Emily Wetherholt, PharmD, BCACP, lives in Schaumburg, Illinois, with her husband, three active children, and dog. She is passionate about advancing the cause of pharmacists everywhere, serving on the Illinois Pharmacist Association Board of Directors. When she isn’t advocating for pharmacy, you can find her exercising with her Fit4Mom friends. Dr. Wetherholt was a 2022–2023 Op-Med Fellow.
Image by Pandagolik1 / shutterstock