The call came at the end of a long day admitting patients as a resident physician. When I answered, expecting to hear my mom's voice, I was instead met with the tone of an EMT: "We were called to your family's house and are currently doing CPR on your father.” In the background, I could hear my mother crying, her voice desperate. I sat paralyzed in the workroom, staring at a half-written HPI.
"Sir, I'm a resident physician," I responded, voice cracking despite myself. "Please just give me the details."
He explained further. My dad had been found passed out in the bathroom and wasn't breathing. They had already shocked him twice without success. The EMS responder tried to reassure me, saying, "We'll take care of him and keep you updated." The call ended. My dad had coded at 52 and I remained in shock, room spinning, tears blurring my vision, not knowing if the next moment they would be calling with a time of death.
The hours that followed were a blur. My younger brother asked, "Will Dad be OK?" and I had no answers for him, just as I had no answers for myself. My family wanted me to be more than a son or a brother; they needed me to be a physician. My medical training couldn't protect me from the sense of helplessness and shock. This was the first time I truly felt the burden of being a physician.
As the hours wore on, we found out more. My dad had suffered a proximal LAD STEMI — the "Widowmaker." He had been resuscitated at home for 32 minutes before he was stable enough for transport. He was intubated and sedated, and they were planning to transfer him to a second hospital for ECMO. This was a story I had heard countless times with patients. But this wasn't a patient — this was my dad. Just hours earlier, we'd been on FaceTime talking about his upcoming visit to see me. Now he was in the ICU, unconscious. I understood the prognosis as a physician, but as a son, I couldn't bring myself to accept it. "It'll be OK," I told my mom and brother, though every instinct inside me warned otherwise.
For the first time, I was on the other side. I watched EMS roll my dad into the unit and quickly glanced at his hemodynamics as they told me to wait outside. In the waiting area, I wiped away my tears, put on a brave face, and went to greet my mom as she arrived. I hugged her tight, her tears flowing freely while I kept mine in. Later, I found a bathroom stall and let myself cry once again.
For hours we sat vigil in that waiting room. Eventually, the cardiology attending called us back for an update. I had kept my jacket on, the one that bore the name of the academic medical center where I trained, because I wanted him to speak to me plainly, doctor to doctor.
“He is stable from a cardiac standpoint,” he explained. "The real concern is his neurological status, since he was without oxygen for approximately 32 minutes." My mom and brother turned to look at me as soon as he said it. I didn't want to tell them what I knew — that this was grave. They wanted reassurance from me, and all I could do was echo the hope the doctor had provided, that maybe there was a chance.
The next days and weeks were a blur. Most of the time, I found myself functioning as a physician. At the hospital, in front of my family, in front of our community, I wore the mask of the medical professional. Only in the privacy of a bathroom stall did I let myself break down, feeling the full weight of my fear and grief. I was my dad's advocate, catching every oversight — a missed arterial clot in his hand on my daily physical exams, drug-induced liver injury from the many sedatives and anti-epileptics, a nurse calling to say he was likely brain dead due to "posturing," prompting me to rush to the hospital, examine him myself, and verify with the attending that his brain stem reflexes were still intact. I couldn't rest, because I watched things get missed and I couldn't afford to lose him due to an oversight.
Eventually, the decision was made to transfer him again. This hospital told us he was brain dead, but that did not make sense to me. There had been too many missteps and I couldn't trust the team anymore. It was a terrible feeling, feeling betrayed by the very system I trained and worked in. My dad's heart was doing well — he had been off pressors and the balloon pump for days — but it was his brain we worried about. I was urged to transfer him by many previous mentors and physicians I was lucky to have access to. Insurance initially denied the transfer, but I used every connection, every tool I had at my disposal to get it approved.
Once transferred, things began to improve slowly. Within a few days, he was off all sedatives and antiepileptics. The team at the new hospital saw no evidence of seizure activity. On Day 31, I received a call from my mom. He was crying. I could see it. It was the first time he had shown any emotion, any awareness. The whole team agreed: this was a sign, proof that he was still in there, still fighting. Dad was in there, in that body now so emaciated, trach in place. He was almost unrecognizable. But for the first time, I had real hope.
On Day 40, he was discharged from the ICU. On Day 43, he was sent to a long-term acute care hospital. On Day 51, I saw my dad again — awake, aware. On Day 55, it was time. Time to explain why he was in a hospital bed, unable to move or speak, with a tube in his neck. Tears streamed down both our faces. I promised him that we were in this fight together, and that we would do everything in our power to help him down this difficult road ahead. Seeing him like this was at times harder than seeing him in a coma. Seeing how hard the smallest things were for him now pained me. But, I was thankful. Thankful because I still had Dad.
In the time since, my dad has continued to defy the odds. Now, a year later, he is walking with a cane and working with a trainer to get stronger. He can talk to us, although his voice is very different due to vocal cord damage from the intubation. But it's him. He made his first trip out to LA to visit me. And he's already set his next goal, to jog a 5K. Every small milestone is a testament to his resilience and the dedication of my family, the health care workers, and our community.
My family and to a certain extent, myself, have developed a mistrust in the system. Every appointment includes me on the phone; every decision comes through me. I consult my colleagues for every choice. Is this healthy? No. But when your trust is broken by the institutions you hold dear, relearning to let go and move past that trauma is a feat that takes time. This experience showed me that doctors can be wrong, myself included. We're not perfect, but when we're wrong, it's not just a patient. It's someone's dad, someone's husband, someone's brother. I was fortunate to be able to advocate for my dad in a way that most cannot and it has made me more diligent with every patient I see.
Sometimes, we anchor on a story that seems to explain everything — like 32 minutes of resuscitation after an out of hospital cardiac arrest — but miss what doesn't fit. There was no evidence of ischemic insult on any of his brain imaging. His initial clinicians were so convinced, he was being described as a rare case. When things don't add up, we must look further. Our decisions can seem small in the moment as we click around in the EMR placing orders, but have such far-reaching consequences. Getting told my dad was brain dead, by multiple physicians, was devastating. We assume the role of God as physicians, making the decision if someone lives or dies, and we owe it to our patients to have all the evidence before we make that call.
But most importantly, this experience has taught me the true depth of my own resilience, as well as my father's. I've seen firsthand how powerful hope can be. I used to think of hope as something fragile, almost foolish, in the face of clinical evidence. But I've learned that hope is what keeps us moving, especially when the odds seem insurmountable. It's what makes us fight for the people we love, what pushes us to question, to advocate, to never give up.
I continue my work as a physician with a different outlook now. When I walk into a patient's room, I remember what it was like for me, sitting across from my dad's medical team, hoping they could take away my fear. And I do my best to provide that kind of care — the kind that's more than medical expertise, the kind that understands what it's like to hope against hope, to fight for every inch of progress. This journey with my dad, while one of the most painful experiences of my life, has also been a reminder of why I chose to become a doctor in the first place: to be there for people in their most vulnerable moments, to be the steady hand that they can hold on to, and to always keep hope alive, even in the darkest of times.
Jay A. Shah, MD, is a third-year internal medicine resident at UCLA and will serve as one of the program’s chief residents for the 2025–2026 academic year. He is passionate about medical education, providing humanistic patient care, and advancing research on South Asian cardiovascular disease. Outside of medicine, he enjoys biking, drone photography, and music. He posts at @JayShah_MD.
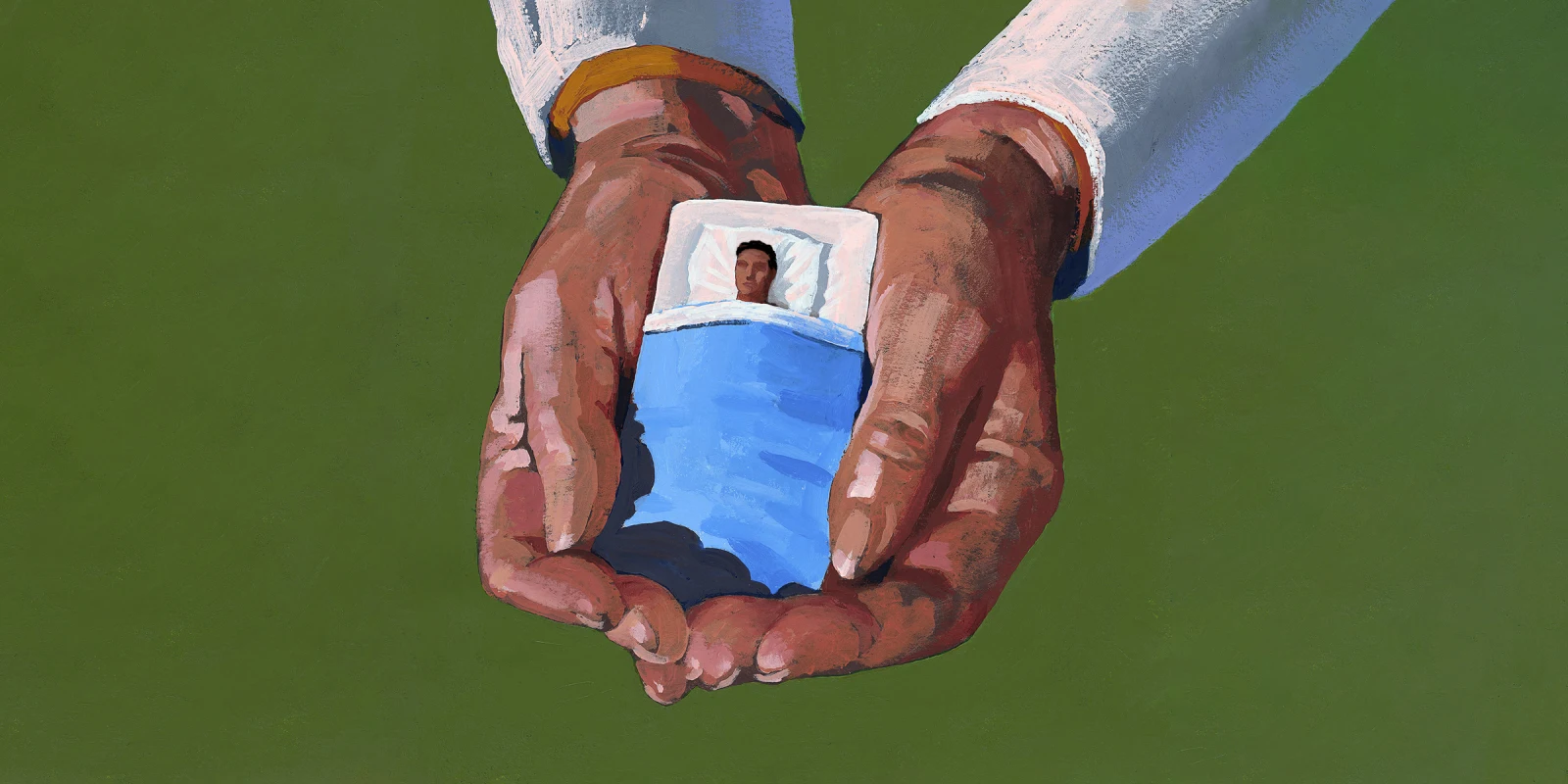
Image by Jonathan Evans / Getty