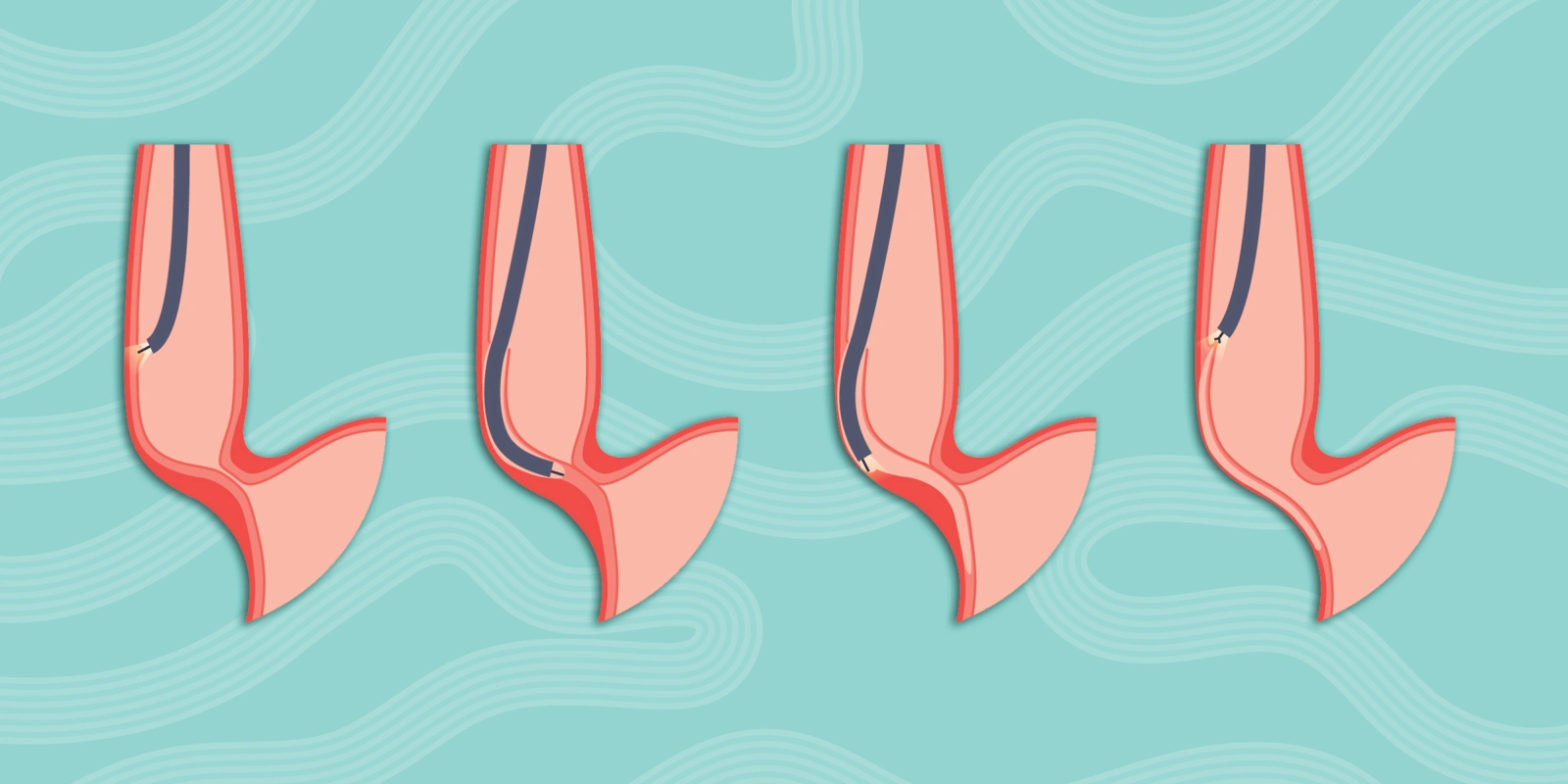
POEM is the iconic procedure that launched an entirely new field of advanced endoscopy, often called “third-space endoscopy.” A recent historical review recounts, in detail, POEM’s unveiling to the world 16 years ago at DDW 2009 in Chicago. POEM has rapidly become the new gold standard in achalasia therapy, largely displacing the more invasive Heller myotomy. In this brief report from DDW 2025, which just concluded in San Diego on May 6, we review emerging POEM research focusing on long-term POEM outcomes, emphasizing the increasingly reported phenomenon of blown-out myotomy (BOM) diverticula. We focused our review on data from submissions selected for oral presentation, a distinction reserved for the highest quality submissions. Two such presentations offered comprehensive POEM follow-up data that included rates of BOM diverticula.
The Italian group from Humanitas Hospital presented their long-term POEM outcomes in 595 POEMs performed from 2012-2024. They noted that 50 (8%) of their POEM patients developed a BOM (which they termed “post-POEM septum”). In 60% of patients, this occurred within the first year after POEM, and 19 of these 50 patients (38%) had high dysphagia scores (Eckardt score>3) consistent with a failed POEM compared to only 10% of non-BOM patients. The investigators noted that 74% of these patients had “anterior” POEM, which may be mechanistically important in BOM formation.
In a much smaller series, the Northwestern group had previously published a similar rate of BOM after POEM (9.4%), which was significantly lower than the BOM rate after Heller (26%) and more frequent among manometric type 3 patients. Similar to the Italian group, they found that these patients had higher dysphagia scores (ES of five in BOM patients versus two in non-BOM patients).
Recently, a European study raised concern as it reported a much higher post-POEM BOM rate of 31% at five years. They also found BOM to be more prevalent among type 3 patients. We should note that this group reported their technique as the “Inoue technique,” the original version of which was an “anterior POEM” technique. Furthermore, their myotomy length was longer than a modern POEM technique (12-13 cm in type 1/2 patients and 17 cm in type 3 patients), and they had a high failure rate (22% of POEM patients required salvage within the first five years).
A recent in-silico model study suggested that long myotomy and incomplete Lower Esophageal Sphincter (LES) myotomy (failed POEM) are critical factors in BOM formation. Regarding the “anterior” POEM orientation, in a personal communication at this year’s DDW with Dr. Haruhiro Inoue (the thoracic surgeon from Japan considered the father of POEM) he raised concern that reports with high prevalence of BOM after POEM may come from centers performing lateral POEM, because laterally the esophagus is least bolstered by adjacent structures as it abuts the lungs which are also subject to negative intrathoracic pressure during inspiration. The weakened (myotomized) and unbolstered lateral esophageal wall and the high-pressure gradient (high intra-esophageal prandial pressure due to inadequate lower esophageal sphincter (LES) myotomy augmented by negative intrathoracic pressures during inspiration) appear to be the two sine qua non’s for a blown-out-myotomy. Therefore, performing a shorter POEM posteriorly at 5-6 o’clock (our favored technique and that of others) may be less likely to result in a BOM compared to a right lateral myotomy at 2-3 o’clock (usually described as “anterior” POEM) or a left lateral myotomy at 7-9 o’clock (typically described as “greater curvature” POEM). Of course, ensuring a complete LES myotomy (adequate extension into the cardia) is also essential.
These conclusions are also supported by the oral presentation from our group of long-term outcomes in 787 consecutive POEMs performed from 2009 to 2021 and enrolled into a comprehensive annual follow-up program, with only 10% of patients missing follow-up within a year of this most recent analysis (November 2024). POEM clinical success was 96% at five years and 92% at 10 years. Prior myotomy (Heller or POEM) was the only predictor of POEM failure on multivariate Cox regression analysis (HR 2.6, P=0.01). Overall clinical success was 95% at a median of 6.4 years, with only 38 failures (20 early failures at a median of 14 months after POEM and 18 late failures at a median of 57 months after POEM).
For the early failures, the leading causes were incomplete myotomy (10) (inadequate extension into the cardia, an early learning curve error) or incorrect myotomy (three) (e.g., opting not to myotomize a proximal esophageal spastic segment, or preserving the LES in Jackhammer or DES patients). For the 18 late failures, however, the leading cause was BOM diverticula (8 cases, or 1% of all POEMs). Only half of the BOM cases were due to the index POEM, with the other half secondary to a failed Heller preceding the POEM. All four BOMs due to POEM were in manometric type 3 patients who had a long anterior POEM, whereas three of the four post-Heller BOM patients were manometric type 2, with only one being type 3.
Interestingly, the DDW presentation by the Italian group suggested an association with achalasia type 2. We could speculate that type 2 achalasia may lead to BOM if there is inadequate LES myotomy during POEM (causing high pressures in the esophagus). Type 3 achalasia could produce BOM even in patients with adequate LES myotomy via high pressures produced by spastic contractions within the esophagus. The very low BOM rate in our series is likely the result of favoring a posterior approach and having shortened our myotomy to 5-7 cm for type 1/2 patients and 10-11 cm for type 3 patients. In terms of BOM management, the Italian group provided salvage therapy in 53% of patients with dysphagia due to BOM: eight redo POEM, two Pneumatic dilation (PD). Our group provided salvage in the eight patients with BOM: four redo POEM+diverticulotomy, three redo POEM, and one from PD. Notably, we also submitted a video to DDW with the novel technique of Per-Oral Direct Diverticulotomy (PODD) Technique, which is our current preferred salvage technique in patients with BOM diverticula. The video was uploaded at the DDW ASGE learning center and is available at the ASGE online educational library (GI Leap). An author’s link to the video is also provided here for readers without access to these resources: Video of our Per-Oral Direct Diverticulotomy technique for BOM diverticula (The video has also been submitted to VideoGIE, an open-access online journal).
Other notable findings in the comprehensive 15-year follow-up of our 787 POEMs included:
- Low rates of esophageal cancers, with a total of 3 cancers (0.4%). All in patients with long-standing achalasia (13-30 years). 2 incident squamous cancers at one and two years post-POEM, treated with esophagectomy; and one prevalent adenocarcinoma found at the time of POEM referral and treated with Endoscopic Submucosal Dissection before POEM.
- Low rate of esophagectomy, seven (0.9%), all in patients with long-standing disease, with 6/7 having end-stage disease at the time of POEM, and 6/7 having had prior failed Heller (five) or POEM (one) before the index POEM
- Low rates of long-term GERD sequelae: 2.7% developed pectic strictures (all due to PPI non-compliance) easily managed with dilation and PPI resumption; 3.7% had Barrett’s at time of POEM and 4.2% developed incident Barrett’s after POEM (PPI non-compliant patients, all short segment without dysplasia/cancer); 1.9% had anti-reflux endoscopic or surgical procedures (all in our earlier conventional POEM period before our technique of sling-preserving anti-reflux POEM starting in 2018)
- Excellent long-term survival after POEM with no deaths related to POEM. 94 (12%) patients died during the 15-year study period. These were older patients with comorbidities, with the median age at time of POEM of 80 and at time of death 85.
In summary, POEM outcomes at 10+ years remain excellent, but the issue of BOM merits attention, particularly among type 3 patients and in centers that favor longer “anterior” myotomy. Shorter posterior myotomy technique appears to be protective with very low BOM rates <10%. The novel PODD technique offers a straightforward management approach for BOM diverticula causing dysphagia.
Dr. Stavropoulos has no conflicts of interest to report.
Image by Pikovit / Shutterstock