Approximately 32,000 people are diagnosed with multiple myeloma (MM) every year in the U.S. Although still considered incurable, there has been a steady improvement in the outcome of patients in recent years, with median overall survival (OS) approaching almost a decade or longer in standard-risk disease that constitutes approximately 85% of newly diagnosed patients. This improvement can be attributed to a better understanding of disease biology, optimal use of autologous hematopoietic stem cell transplant (auto-HCT), availability of several novel treatments, advancements in supportive care, and development of immune- and cellular therapies.
Stem Cell Transplantation
High-dose chemotherapy followed by auto-HCT remains the standard of care for transplant-eligible, newly diagnosed patients since the 1990s, based on the results of several randomized phase III trials showing an improvement in the depth of response and progression-free survival (PFS) with upfront auto-HCT. Updated results from several large randomized phase III trials presented at the recently concluded ASH Meeting validated its continued benefit. In one trial, the FORTE trial, Italian investigators reported the outcomes among three groups: a) induction therapy with four 28-day cycles of carfilzomib, lenalidomide and dexamethasone (KRD) followed by auto-HCT, and then consolidation with four cycles of KRD; b) continuous treatment with 12 cycles of KRD; or c) induction therapy with four 28-day cycles of carfilzomib, cyclophosphamide and dexamethasone (KCD), followed by auto-HCT, and then consolidation with four cycles of KCD. Thereafter, patients were randomized to maintenance treatment until progression with either KR or R. Primary endpoint was progression-free survival (PFS). The trial enrolled 474 patients divided between three arms. After a median follow up of 45 months, there was a significant improvement in PFS in the KRD-auto-HCT arm (not reached versus 57 and 53 months, in KRD 12 and KCD arms, respectively). Furthermore, maintenance with KR also showed an improvement in PFS compared to R alone.
Another study from the European Myeloma Network (EMN02/HO95) reported an update after an extended follow up of 75 months in 1,197 patients, who received either a) auto-HCT (702) or b) consolidation a combination of bortezomib, melphalan, and prednisone (VMP: 495). They had previously shown a 15-month improvement in PFS with auto-HCT versus VMP (57 versus 42 months) in an article published in Lancet Haematology earlier this year. In this updated report, they showed that auto-HCT significantly improved the OS (69 versus 63%), and the time to next line of treatment (66 versus 47 months), both meaningful clinical outcomes. The benefit of auto-HCT was seen across the board, including in patients with advanced stage disease, and high-risk chromosomal abnormalities at diagnosis.
These results emphasize the importance of upfront auto-HCT in newly diagnosed MM in all transplant-eligible patients. However, auto-HCT is significantly underutilized in the U.S., with only about 40% of transplant-eligible patients actually receiving this therapy. As a safe, effective, and relatively economical therapy that offers durable remission across all subgroups, auto-HCT should be more commonly used for newly diagnosed MM patients.
CAR-T Cells
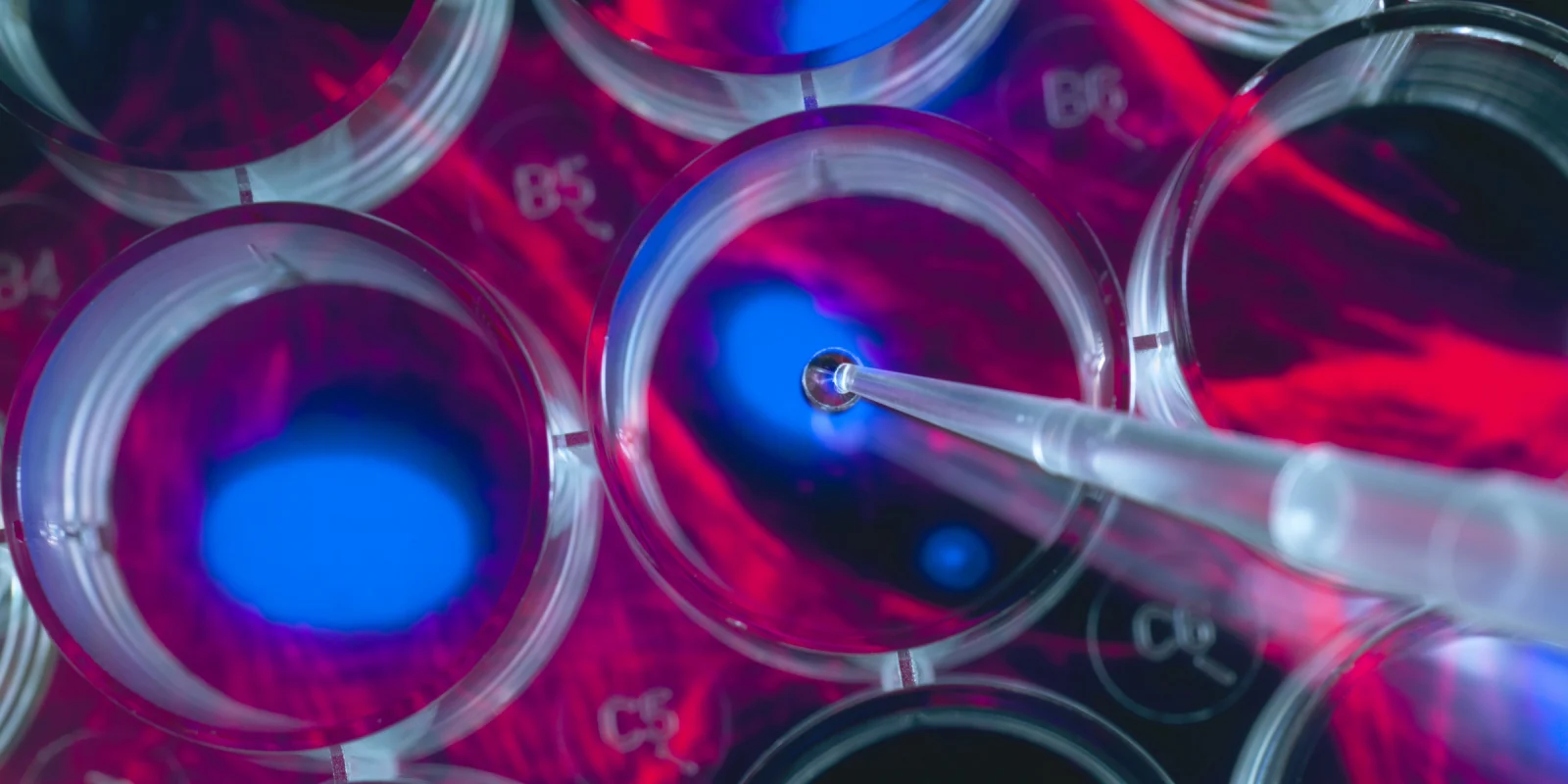
The last decade has seen an explosion of immune-based therapies that have revolutionized cancer care worldwide. One of these therapies, CAR-T cells, uses patient’s own T lymphocytes that are genetically engineered to express a chimeric antigen receptor (CAR). CAR is a synthetic molecule designed to target a protein (antigen) on the surface of tumor cells. Two different CAR-T cell products targeting CD19 antigen on the surface of B cell malignancies were approved by the FDA in 2017. So far the greatest success of CAR-T cells in MM has been in targeting B cell maturation antigen (BCMA) that is expressed on the surface of malignant plasma cells. Ide-cel and ilta-cel are the two CAR-T products in the most advanced stages of development. A number of clinical trials presented at ASH 2020 highlighted the continuous growth and evolution of this approach.
Some common themes have started to emerge for CAR-T cells in MM. Almost all these trials involve the use of patient’s own (autologous) T cells. Patients receive lymphodepleting chemotherapy, most common being a combination of fludarabine and cyclophosphamide, given over three days, before the CAR-T cell infusion. A disarmed lentivirus or retrovirus is used to genetically modify these T cells to express CAR on their surface. All the trials presented at ASH 2020 used BCMA as the target antigen and were conducted in patients with relapsed or refractory MM that had progressed despite multiple prior lines of therapy, and included patients with advanced, high-risk, and bulky disease. Median follow up for most of these trials has been short, with the longest follow up stretching to almost 15 months.
These studies showed unprecedented response rates, ranging from 55 to 95% after a single CAR-T cell infusion. Overall, the observed responses were short-lived, and the median response duration was less than a year. CAR-T cell therapy is marked by unique and potentially life-threatening toxicities. In addition to almost universal cytopenia due to the myelosuppressive effect of lymphodepleting chemotherapy, these treatments produce cytokine release syndrome in 70–90% of patients, mostly low-grade and reversible after treatment with anti-IL6 drugs or steroids. ICANS (immune effector cell-associated neurotoxicity syndrome) is another distinct toxicity with CAR-T cells, reported in 20-40% of treated patients, also reversible with steroids.
Even with these promising results, CAR-T cells face substantial challenges in the future. Innovative research is already underway to improve the durability of response, enhance the safety, and to improve the manufacturing, distribution, and accessibility of this groundbreaking treatment.
References:
- Autologous Transplantation for Newly Diagnosed Multiple Myeloma in the Era of Novel Agent Induction: A Systematic Review and Meta-analysis. B Dhakal et al.
- JAMA Oncol. 2018 Mar 1;4(3):343-350.
- Future of CAR T cells in multiple myeloma. K Wudhikarn et al. Hematology Am Soc Hematol Educ Program 2020 (1): 272–279