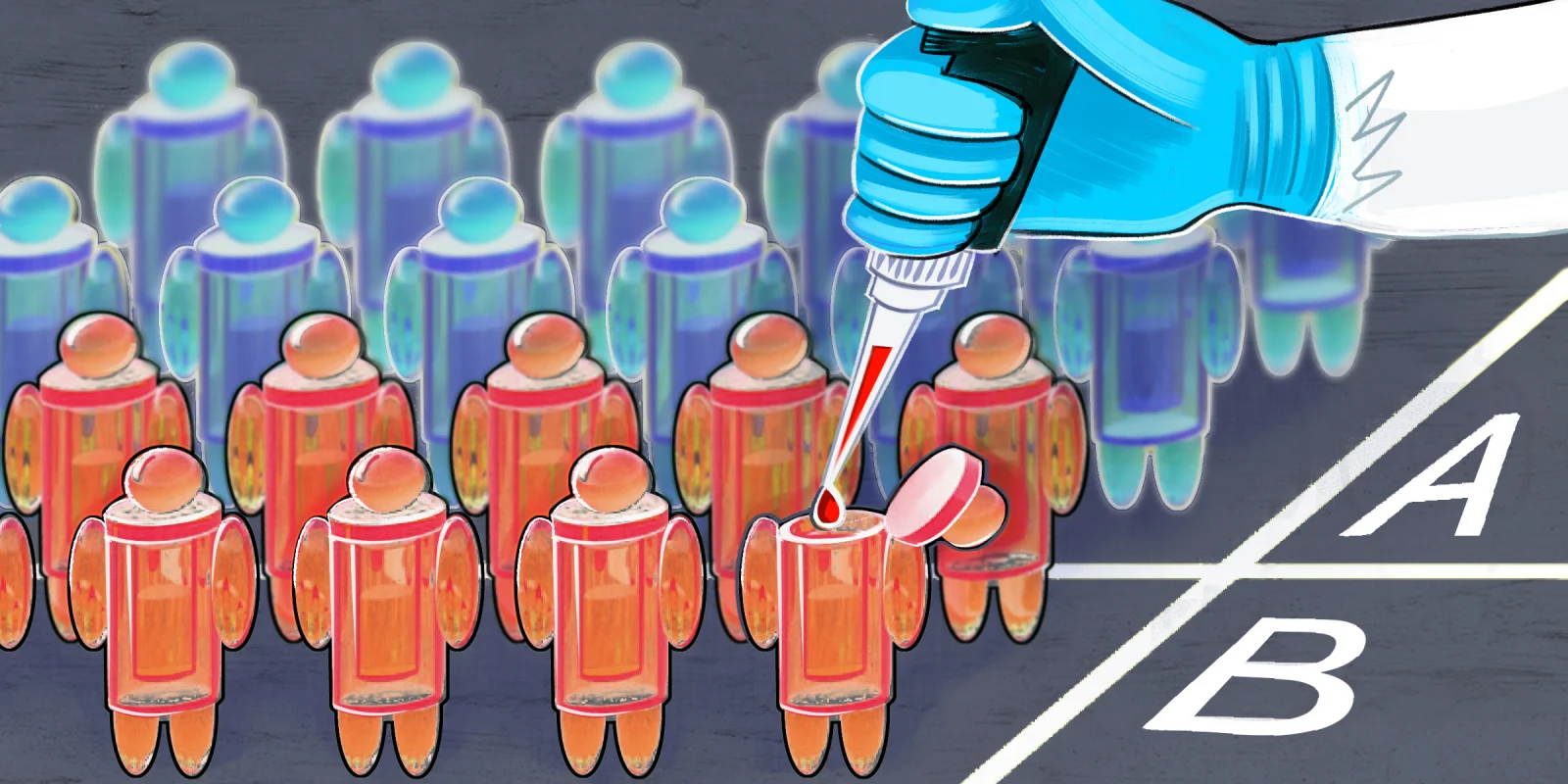
ASCO Voices continues to be one of the most powerful sessions of the annual meeting. The meeting theme changes yearly, this time emphasizing patients as the cornerstone of cancer care and research. However, the lack of access to clinical trials for many results in low enrollment and a trial population not representative of the majority of real world patients with cancer, a continuing issue, as in years past.
“Change has been slow,” according to Rajasree Pia Chowdry, MD. “Cancer care is still segregated, and those patients who need clinical trials the most have the least access to them.” These include those who can’t afford gas money to get to the clinic, those diagnosed with rare tumors at a young age, and those, like her patients, who live in Cancer Alley in Louisiana. “It should be our duty to bring clinical trials to them, not the other way around,” she said.
Dr. Chowdry offered suggestions to increase access and diversify clinical trials, including designing a mobile clinical trials unit that prioritizes underserved areas with high cancer rates, leveraging technology to enroll patients virtually (so distance no longer has to be a barrier), and increasing funding to critical access safety net institutions so that they can remain open and create community outreach programs to educate patients on the value and importance of clinical trials.
Although there are places where some form of these measures have been implemented, Dr. Chowdry said that there needs to be a cultural change and a paradigm shift in the oncologic research landscape. “Cancer statistics won’t change unless we ensure equitable access to all. All the incredible advances in oncology are meaningless if we can’t help the people who need it the most.”
Samantha Siegel, MD, had taken care of her physician husband through his own cancer, liver transplant, and colectomy, only to be diagnosed with Hodgkin’s lymphoma herself. She described the realities of treatment in detail, including the side effects of chemotherapy and the grueling autologous transplant after her lymphoma recurred.
Now in remission and almost finished with post-transplant therapy, she said, “I want you to see us patients for the whole people that we are, in the context of our lives, for the incredible lengths that we have to travel just to stay here. I want you to know that getting cured and healthy are not the same.”
Switching her focus from internal medicine to integrative medicine, Dr. Siegel’s dream is to build a comprehensive cancer survivorship program which justifies the need for a distinct, board certified specialty dedicated to those living with and after cancer.
“Patients need a roadmap for recovery, because the healing continues well after a clean or stable scan gives permission to go on living,” she said, noting that surveillance is not survivorship. “I’m proudly a doctor, but I’m a patient now, too,” she concluded. “The line is forever blurred.”
Dr. Lederman has no conflicts of interest to report.
Illustration by April Brust