The 2021 Gastrointestinal Cancer Symposium was clearly like no other, as the past year has been. To their credit, the organizers of the Symposium have learned from other meetings that were forced to shift to a virtual meeting format, and I think this meeting allowed more interaction with presenters than other meetings had, and allowed an experience much closer to the usual. One of the best elements of the GI Cancer Symposium, and something that distinguishes it from the annual meeting, is its multidisciplinary nature. While we always hope to learn about groundbreaking new studies and developments, often those results are presented at the annual meeting. However, this meeting’s size and focus on GI malignancies allowed better discussions about vexing clinical issues with a particular focus on multidisciplinary approaches, and how to interpret and build upon study results, especially as the GI Cancer Symposium occurs six months after the ASCO Annual Meeting and three months after the ESMO meeting. Thus, there is plenty of time to digest the new studies that are presented there, and understand how to integrate them with our current paradigms, or better consider how best to further progress that has been made.
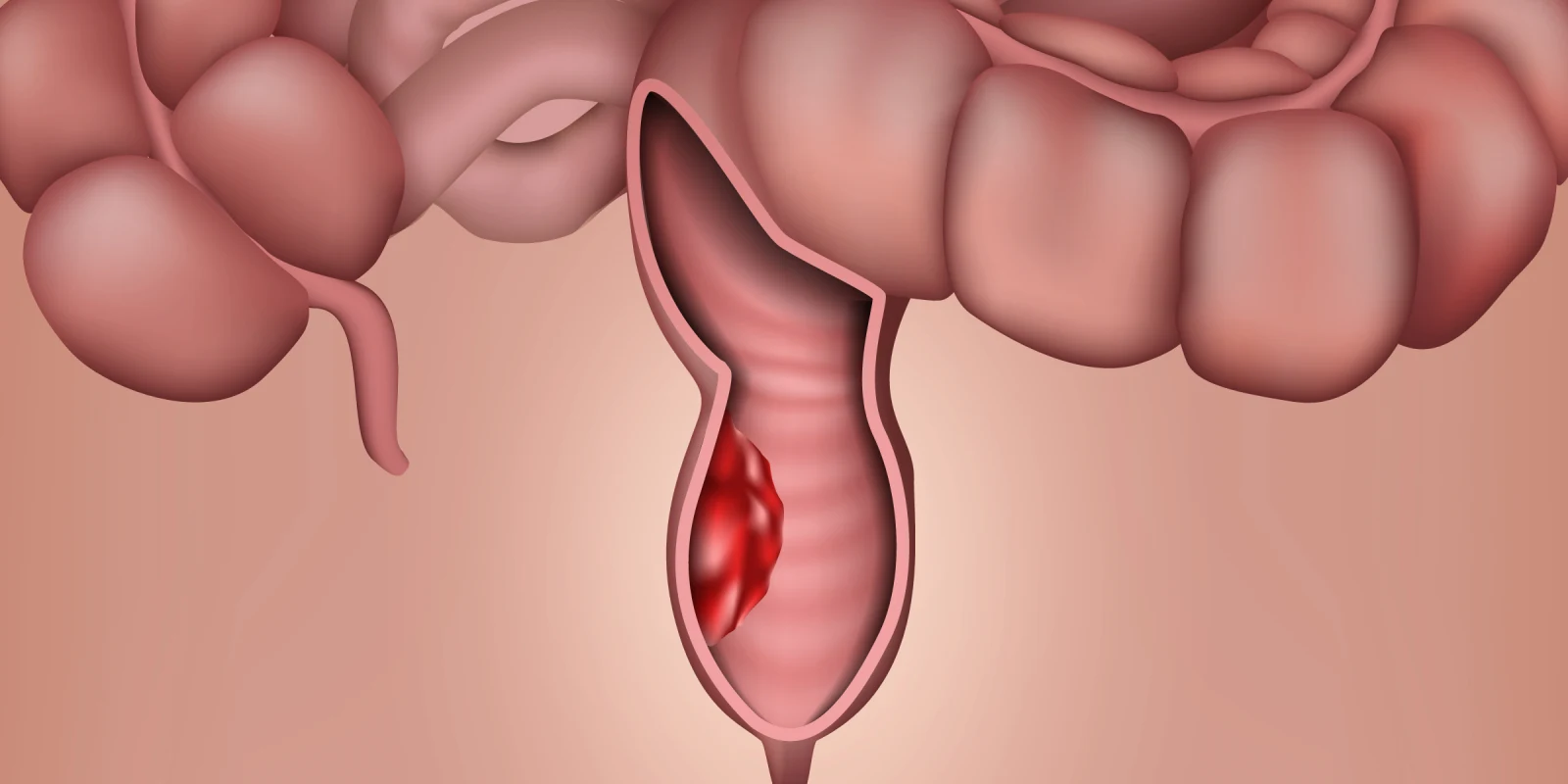
This year’s GI Cancer Symposium focused my attention on the perioperative and potentially nonoperative approaches in rectal cancer. While there is still no agreement about a single best management pathway, there did seem to be an emerging consensus that both short course radiation and systemic chemotherapy, or more traditional long course radiation with concurrent fluoropyrimidine, as demonstrated in the RAPIDO study (Bahadoer et al, Lancet Oncology 2021, 22: 29-42) are appropriate neoadjuvant approaches in rectal cancer. The NACRE study reported by Francois (abstract 4) reprised this study design, with a shorter period between radiation and surgery in the short course arm, and no systemic therapy interposed, in 104 patients who were 75 year of age and older. There was no difference in R0 resection rate, or disease free survival. While survival estimates were somewhat premature, the survival rate at six and 12 months favored the short course of radiation. However, these options are not necessarily fit for all patients, with the long course radiation perhaps more favorable for lower tumors, though the short course radiation followed by chemotherapy may yield a higher chance for pathologic complete response.
A burgeoning body of results from prospective randomized studies has buttressed our understanding of initial chemoradiation, followed by “watch and wait” approaches in rectal cancer. Supporting the OPRA study presented at the 2020 Annual Meeting by Dr. Garcia-Aguilar (abstract 4008), Myint presented the results of the OPERA study (abstract 12). In the OPERA study, 148 patients with cT2-3 rectal adenocarcinoma by MRI, 5 cm or smaller, and within 12 cm of the anal verge were treated with 45 Gray XRT with concurrent capecitabine, with half randomly assigned to receive contact brachytherapy as a boost. Eighty-one percent of patients had a clinical complete response, and at 19 months, 34% of the evaluable patients underwent surgery, including TME surgery in about 20% of patients. The results by treatment arm were not yet available. Longer follow-up is necessary, but certainly these results suggest that surgical resection may not be necessary in all patients with rectal cancer. However, enhancing our ability to predict who those patients are is the key.
Katz presented the results of the Alliance A021501 study (abstract 377), a randomized phase II trial which was conducted in patients with borderline resectable (by Intergroup Definition) pancreatic adenocarcinoma. There were 126 patients who enrolled in the study. They were randomly assigned, initially to modified FOLFIRINOX x 8 or mFOLFIRINOX x 7, followed by stereotactic body radiation S(BRT), surgical resection. The mFOLFIRINOX/SBRT arm did not meet the prespecified benchmark for efficacy R0, whereas the mFOLFIRINOX arm did. Moreover, survival and disease-free survival favored the FOLFIRINOX arm as well. Therefore, FOLFIRINOX will represent the reference standard neoadjuvant therapy in the Intergroup for borderline resectable pancreatic adenocarcinoma. However, this still does not represent the last word in the management of this patient population, as it may be argued that perhaps a longer course of radiation with concurrent capecitabine may be more effective than SBRT for neoadjuvant therapy, in particular with regards to resection margin.
As always, my attention also went to some potential new therapeutic directions in the treatment of advanced diseases. The area of almost perpetual interest is the evaluation of immunotherapy in patients with advanced metastatic microsatellite stable colorectal cancer. Several studies focused on continued PD1/PDL-1 inhibitors with antiEGFR antagonists (Lee, abstract 7; Van Der Eynde, abstract 80); and antiVEGF therapy (Bocobo, abstract 77; Gomez-Roca, abstract 94), with modest effect including response rates about 10%.
In addition, on the heels of the IMBrave 150 study (Finn et al, N Engl J Med 2020; 382: 1894-1905) that demonstrated the superiority of atezolizumab and bevacizumab over the prior standard of sorafenib, there was some discussion and initial reports exploring potential second line approaches in this setting. These included a retrospective evaluation of the addition of the antiCTLA4 inhibitor ipilimumab from Hong Kong, (Wong, abstract 330), with a response rate of 16% in 25 patients.
Perhaps the most exciting presentation at the GI Cancer Symposium was Wainberg’s reports on the “FIGHT” study (abstract 160), evaluating bemarituzumab, a monoclonal antibody targeting FGFR2b, in metastatic gastric and gastroesophageal adenocarcinoma. They noted that about 30% of patients screened for the study had FGFR2b overexpression by immunohistochemistry, and were therefore eligible for the FIGHT study, which was conducted in the first line setting. There were 155 patients with advanced gastric/GEJ who were randomly assigned to FOLFOX with or without bemarituzumab. The combination demonstrated increased progression-free survival (median 9.5 months versus 7.4 months with FOLFOX alone, hazard ratio 0.68), survival (HR 0.58, but median follow up was only 10.9 months), and objective response rate (53% versus 40%). As a new therapeutic approach, attention was also paid to toxicities, which included grade 3 stomatitis (9.2% versus 1.5%), and corneal toxicities (23.7%, generally mild). These intriguing results will lead to a phase 3 study, and point to intriguing new avenues of exploration in the increasingly segmented area of gastroesophageal adenocarcinomas.
While the 2021 GI Cancer Symposium experience was a marked improvement over the 2020 ASCO Annual Meeting, I think I speak for many when I say we yearn for the return of in-person meetings, which allowed for greater interaction and discussion of data, which accelerates the understanding and absorption of data. Nonetheless, what I discussed here is only the tip of the iceberg, and there was plenty more new and exciting information to whet our appetite for further advances that lie ahead.
Jimmy Hwang, MD FACP is a chief of GI Medical Oncology at Levine Cancer Institute, Atrium Health in Charlotte, North Carolina.
Image: medicalstocks / shutterstock