This year’s ASN Kidney Week included a thought-provoking series of lectures moderated by Laura Barisoni and Avi Rosenberg with several talks about the implementation of image analysis and machine learning to streamline the process of kidney biopsy interpretation and potentially provide information on disease prognosis as well as guide therapy.
Several examples of the machine’s ability to reliably interpret kidney biopsies were cited – quantification of interstitial fibrosis and inflammation, tubular atrophy, glomerulosclerosis via relatively accurate tissue segmentation, and extrapolating this to assist with BANFF classification. Additionally, some of the studies quantified parameters using frozen sections – traditionally difficult due to the presence of artifacts. Andrew Janowczyk discussed several pre-analytical technological tools to filter out artifacts in a uniform manner and prioritize high-quality slides for expert interpretation. Additionally, algorithms could generate artificial images that are stain-independent, immensely simplifying the nephropathologist’s workflow – but this of course raises a wide set of concerns related to image validity.
Quantifiable pathologic parameters could then be correlated with clinical treatment and outcomes data, and this is where this technology becomes extremely powerful. Several cited studies correlated these parameters with creatinine, GFR, proteinuria, survival, as well as genetic and immunologic data and even psychosocial variables. Additionally, spatial data could be trended over time with large image repositories, allowing for the extraction of clinically relevant longitudinal information with potential prognostic value.
For example, Alton Farris discussed his group’s use of glomeruli identification to bound renal cortex and a positive pixel count algorithm to identify areas of fibrosis, and attempted to correlate these with graft survival. Pinaki Sarder described a correlation between machine-classified glomeruli, tubules and proteomics data in diabetic nephropathy correlated with CKD progression. He found that while urinary features outperformed the other data sets, that tubular features were actually more predictive of disease progression than glomerular features, suggesting that perhaps we should move our focus away from glomeruli and take a closer look at the tubules in deepening our understanding of diabetic nephropathy. In a separate session, Ashish Verma discussed the use of artificial intelligence to identify AKI subtypes which were associated with clinical outcomes and therefore may be a window into prognostic information.
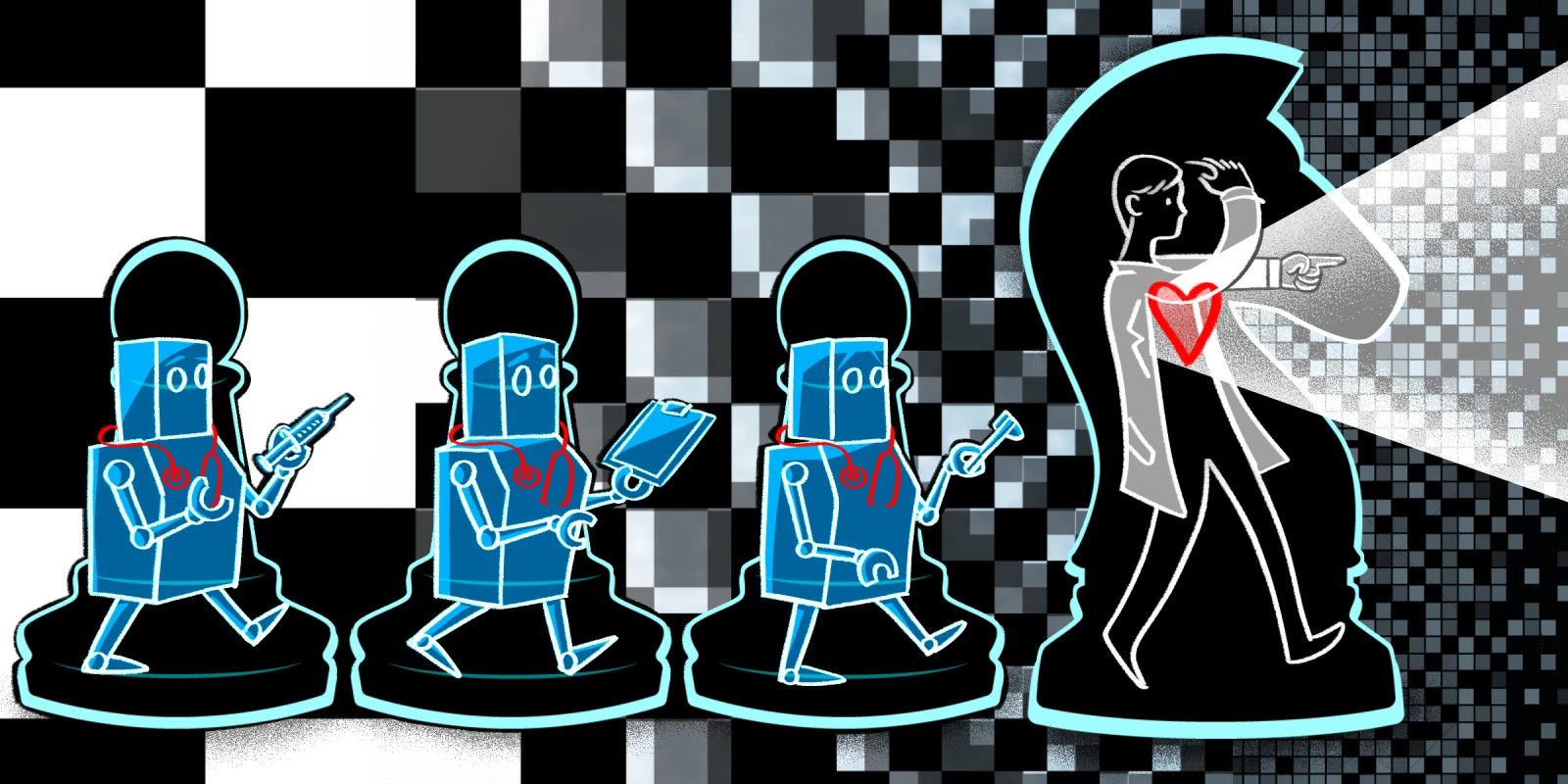
There was a clear elephant in the room amidst discussions of increased reproducibility and uniformity, and increasingly sophisticated trainable algorithms which could pick up patterns that may not be visible to even the most astute nephropathologist. Could these technologies replace expert physician interpretation? And should they?
The consensus opinion was that these advances should not be thought of as replacing the nephropathologist’s role, but rather augmenting it and generating higher-quality data through synergistic efforts. At a very basic level, implementation of artificial intelligence techniques could streamline the nephropathologist’s day-to-day work by taking over lower-order tasks such as counting cells and structures, assigning tissue scoring based on pattern recognition and clinical algorithms, or even ordering stains, freeing up valuable time for higher-order tasks such as the correlation of findings with clinical outcomes as well as other large data-sets related to genetics and immunology. Andrew Janowczyk discussed a tool that could quickly annotate large regions of identical objects which would otherwise require repetitive efforts on the part of the physician, thereby allowing the physician to focus his or her attention more efficiently and meaningfully. In fact, he stated that the results of the algorithm were more precise than the ground truth, suggesting that perhaps the machine mitigated the effects of physician fatigue. He discussed another tool which could identify cohorts with similar features, allowing the physician a larger-scale view of the data set that could then be triaged for closer review.
Furthermore, the issue of data validation was acknowledged by all of the speakers. Validation by human experts is required to train the algorithms – what Pinaki Sarder called the Human-AI Loop. Peter Boor described the security issues associated with differentiating real from artificial images as the technology improves and that deep-learning algorithms can be easy to fool, requiring programmers to build so-called attacks into the machine training models as a potential solution. The artificial images do in fact have a powerful role in strengthening the machine algorithm as well, since they increase the size of the training data set and improve the machine’s performance. Alton Farris interestingly remarked that while it is possible to produce artificially generated slides that the machine may interpret as glomerulosclerosis for example, that these are easily singled out as imposter images by a nephropathologist.
So we aren’t quite ready yet to be taken over by machines - but in a world where the machine may one day see with greater precision and resolution than the human eye to derive unbiased morphological data from histology, how will we keep the machine in check?
A few other concerns were highlighted as well. Peter Boor described a goal of transforming pathology into something more computational and precise, but do we lose valuable interpretation when we filter out specimen heterogeneity with a machine algorithm? If we can only train a machine to look for a finite set of features, do we close ourselves off to discovering what exists beyond those defined confines? And in a world where nephropathologists already do an excellent job in their work, and given the immense initial investment of resources and infrastructure building needed to transition to a workflow model that utilizes artificial intelligence as well as obtain approval from regulatory authorities, will the logistics associated with implementing these technologies become barriers?
Artificial intelligence has already made its way into the arena of nephrology, and while its role is very much still being defined and fine-tuned, its potential application shows immense promise and will continue to evolve even after implementation. Much like other technologies have transformed society and allowed us to achieve greater heights as their gatekeepers, it’s time for us to embrace this technology as well and eagerly look forward to wherever it may lead.
Dr. Rajendren and Dr. Radhakrishnan have no conflicts of interest to report.
Illustration by April Brust