For clinicians working in urban areas, the advent of COVID-19 made circumstances far worse for their patient populations. However, many clinicians viewed it as confirmation of an already broken system. It was during this time that three Detroit NPs began to formulate an idea for a book that addresses key issues in urban health practice from a clinical and practical standpoint.
Since its publication, Urban Health: A Practical Application for Clinical Based Learning, has been downloaded 1,739 times in over 100 countries. Doximity spoke recently with the authors of the book, Cynthera McNeill, DNP, a geriatric NP, Umeika Stephens, DNP, a dual-certified, psychiatric-mental health/family medicine NP, and Tara Walker, DNP, an acute care NP. All three women are also assistant professors in the nurse practitioner program at Wayne State University in Detroit.
Doximity: What lessons did you, as urban health clinicians, learn from COVID-19?
Cynthera McNeill, DNP: As someone from the most affected social demographic — being from Detroit, and working here during the pandemic, — I already understood the pre-existing disparities. I think it allowed individuals living outside urban areas to really see the disparity that was going on prior to the pandemic, and how it increased the number of individuals in underserved communities that were suffering disproportionately related to health outcomes.
Umeika Stephens, DNP: Urban clinicians weren’t surprised that there were huge health disparities, but what people always want is evidence. COVID-19 was the tangible thing that pulled the curtain back on pre-existing issues. Let's leave the curtain back and talk about how we fix these things that we know are broken in health care for people who do not have access to appropriate resources.
Tara Walker, DNP: For me, it was confirmation to every anecdotal thought that I’ve had. But people need the data. What [COVID-19] did is shine a bright flashlight on the racism that exists in health care that people don't want to talk about, because clinicians are supposed to care. Clinicians take an oath to do no harm, yet we saw firsthand that harm was being done, and it was very ugly. It was almost like the Emmett Till moment to see that open casket of what racism was doing in the South. During COVID-19, we saw what racism was doing in health care.
Dox: What advice would you give to clinicians moving forward from COVID-19 on how to deal with the disparities in health care?
CM: One of the reasons why we wrote this textbook was to provide a tool to help educators and clinicians understand some of the disparities in urban communities. I'll give one example. How do clinicians and educators help patients to meet their health goals? We’re quick to say eat healthy food, but you need to consider that patients may have financial constraints that make it difficult for them to do that, and maybe their income leans more towards buying foods that are more filling like a pizza that could feed their family for $5.00. By just telling them they need to eat better, you really haven't done anything because you haven't taught them how to do that in their lived experience of limited resources.
Clinicians should consider patients' resources and provide personalized guidance. This includes teaching them to read food labels, promoting moderation, and informing them about community resources when they can't afford their medications.
US: It’s important to understand the environment of the people you treat. For instance, if you work in a different neighborhood than where you live, make an effort to learn about their experiences and not assume they’re the same as yours. In public health, it’s called a “windshield survey” to drive around the neighborhood. What do you see? One of the things we talk about in the textbook is that we teach from a very middle class, resource-unlimited perspective in health care. We assume that they can get whatever intervention that we talk about.
Then clinicians get upset: “Well, I sent you to the cardiologist, and you didn’t go.”
Patients aren’t readily going to tell you that they can’t afford the $75 copay. You have to be able to ask, “What seems to be the barrier for you to be able to go there? Is it money? Let me know so I can figure out ways to help you.”
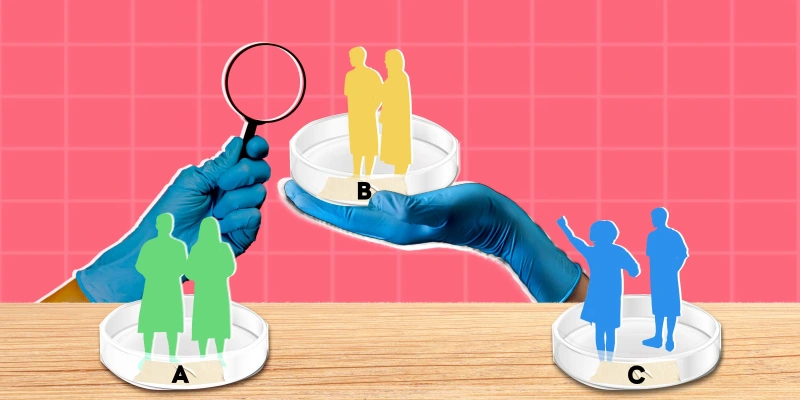
When you meet with your patient, it's a meeting of two experts. You are an expert in whatever health care arena you're in, and that patient is an expert about their life and their lived experience. In order for you both to meet a goal, you need to come to some type of consensus on ways to reach it.
TW: As an acute care nurse practitioner, I see patients when they're in the exacerbation of their disease, or in their first encounter with the health care system. Understanding the social determinants impacting my patients is essential. I balance their immediate health needs with factors like their access to resources. I have to work to complement, not disrupt, their established care plans.
We also need to teach them: “When you call for your follow-up appointment, tell them you were just hospitalized.”
Patients don't realize they get priority that way, and follow-up is important, but because access to care is limited, they often can't get into a primary care appointment for a month. Within that time period, they end up coming back to the hospital, so now we have a 30-day readmission. Hospitals and clinicians need to look at evidence-based interventions that provide comprehensive care and take into consideration the social determinants so that we're stopping that repeat cycle. If they haven’t already established their primary care, we need to work closely with our case managers to make sure that the transition back to the ambulatory setting is very tight and concise.
Dox: One of the chapters in the book discusses medical mistrust, particularly in the African American community. What would you say to a clinician coming into a city, dealing with a primarily Black or LatinX population and trying to gain their trust?
US: Leave your savior complex at the door. A lot of times people have this idea that they're going to come in and save a group of people. Reflect on understanding this community, not whatever stereotypes or preconceived notions that you have about them. Listen, ask questions, listen. I think people are afraid to ask certain questions because they don’t want to be seen as racist. But people can tell the difference when you are inquiring to grow versus inquiring to be judgmental.
You also have to be able to look at other factors. What are the cultural factors that play into this? Is this going to be a group decision? Do they have to go back and talk to their family? You have to understand the context in which successful care delivery is going to happen. Sometimes it's not this traditional individualized focus of care. You have to be able to understand your impact within their community network. And that's not how we train people. We say the patient is the patient, but in certain communities, you have to be able to network within that family. Outreach and volunteering can also aid in understanding the community's needs. It’s important for clinicians not to impose their own ideas of help, but to support individuals in determining what kind of help they need and how they want to receive it.
CM: Clinicians need to acknowledge that some patients have had poor experiences or negative experiences with the health care system, and that medical mistrust is real. It's more than just a historical recount. When people talk about their health care experiences, it is typically from their families that have lived experiences of medical mistrust or poor treatment. So it's more than just the concept of medical mistrust. You have to acknowledge that and value their experience.
Engaging in a genuine manner by familiarizing yourself with their medical history and avoiding repetition of their stories can establish trust. Patients often complain about seeing different clinicians each time, which contributes to medical mistrust. Building a strong relationship and ensuring continuity of care can help bridge this mistrust.
TW: Clinicians really need to check their bias at the door. It is important to treat all patients with equal and respectful care and not take advantage of their trust. Medical mistrust can be exacerbated if clinicians in urban or rural areas do not provide the same level of targeted care as they would in suburban hospitals. It’s important to discard any historical stereotypes or biases, such as assuming that black people, and in particular black women, have a higher pain tolerance. Treatment should be based on the pathophysiology and not on any preconceived notions.
Dox: What advice would you give to clinicians moving forward in the age of private equity medicine?
CM: First, we have evidence-based guidelines to approach patients with chronic conditions. However, these guidelines don't consider social determinants of health. Second, as a health care provider, I'm held accountable for my patients' health outcomes, such as controlling their diabetes and blood pressure. However, patients in urban communities with limited resources face socioeconomic barriers to health care access and struggle to meet goals. This creates unfair penalties for clinicians. The health care system needs a complete revamp to address these issues while still focusing on improving patient experiences today. We must advocate for change on a political level and work within the lived experiences of patients to move forward. This means acknowledging and addressing the health care system's inherent disparities while providing immediate support to the patient based on their lived experiences.
TW: If insurance companies limit reimbursement for Medicaid, we should consider the importance of embracing APPs, particularly in managing routine illnesses. Why should this group of capable professionals be denied the opportunity to take care of such cases? By restricting access, we are only exacerbating the current health care challenges in America. Other countries are outdoing us. If you look at their mix, they use physicians and nurse practitioners appropriately to have better outcomes. A prime example is maternal health care in countries like Norway and New Zealand, which outperform the U.S. by utilizing nurse midwives.
US: In the face of private equity, you should maintain professional accountability, advocate for your patients, and take opportunities to serve on decision-making committees so that advanced practice providers' voices are heard during those decisions. I know that this becomes difficult when you have organizations who are focused on profit over patient care, but we have to remain diligent in our dedication to patients.
Dox: What would you like to see happen in the near future to alleviate some of the more pressing issues for your patients regarding health inequity?
US: We should actively use the knowledge we have gained during the pandemic, as well as continued acknowledgement and development of programs that can address health disparities.
CM: We need better training on working with urban patients, covering various demographics such as geriatric and LGBTQIA populations. We made the textbook an open access resource in the hopes that we can get our colleagues to collaborate with us to build this out more and make it more relatable to other cities like Philadelphia, New York, and Atlanta.
TW: It's crucial to ensure access to primary care and promote preventative health care practices. We need to increase resources and clinicians to meet patients' health care needs and encourage early intervention and education.
Cynthera McNeill, DNP, Umeika Stephens, DNP, and Tara Walker, DNP have no conflicts of interest to report.
Image by DrAfter123 / Getty