I sat amid a research demonstration, computer fans buzzing furiously, a small progress bar loading slowly. I was watching a computer read a 12-lead ECG and determine the diagnosis of the patient. I waited anxiously. Was this the moment we had all been waiting for? The computer spat out a diagnosis: “normal sinus rhythm.” I was stunned. Throughout the demonstration, the machine had correctly identified this case and several others with different pathologies based on the 12-lead ECG alone. I examined the next system, which was designed to read chest X-rays. Here again, the computer correctly identified diagnoses of pneumonia, broken ribs, or cardiomegaly. I sat around with the group of engineers who were buzzing with excitement. However, all I could think was, Am I going to have a job in the future?
Artificial intelligence (AI) and machine learning have become household terms for anything that uses specialized computer systems and massive amounts of data to predict outcomes based on input measurements. Most people know AI from their Netflix account, one of the first consumer-level AIs to use specific “people characteristics” to suggest new shows to watch. AIs have become exponentially more powerful and more sophisticated since then, and are solving more complex problems. One of the most challenging tasks for an AI is competing with humans in video game environments. However, recently, AI has begun to completely dominate this field, winning games with a near-perfect record against some of the best game players in the world. Not to mention, you can never beat your phone at chess.
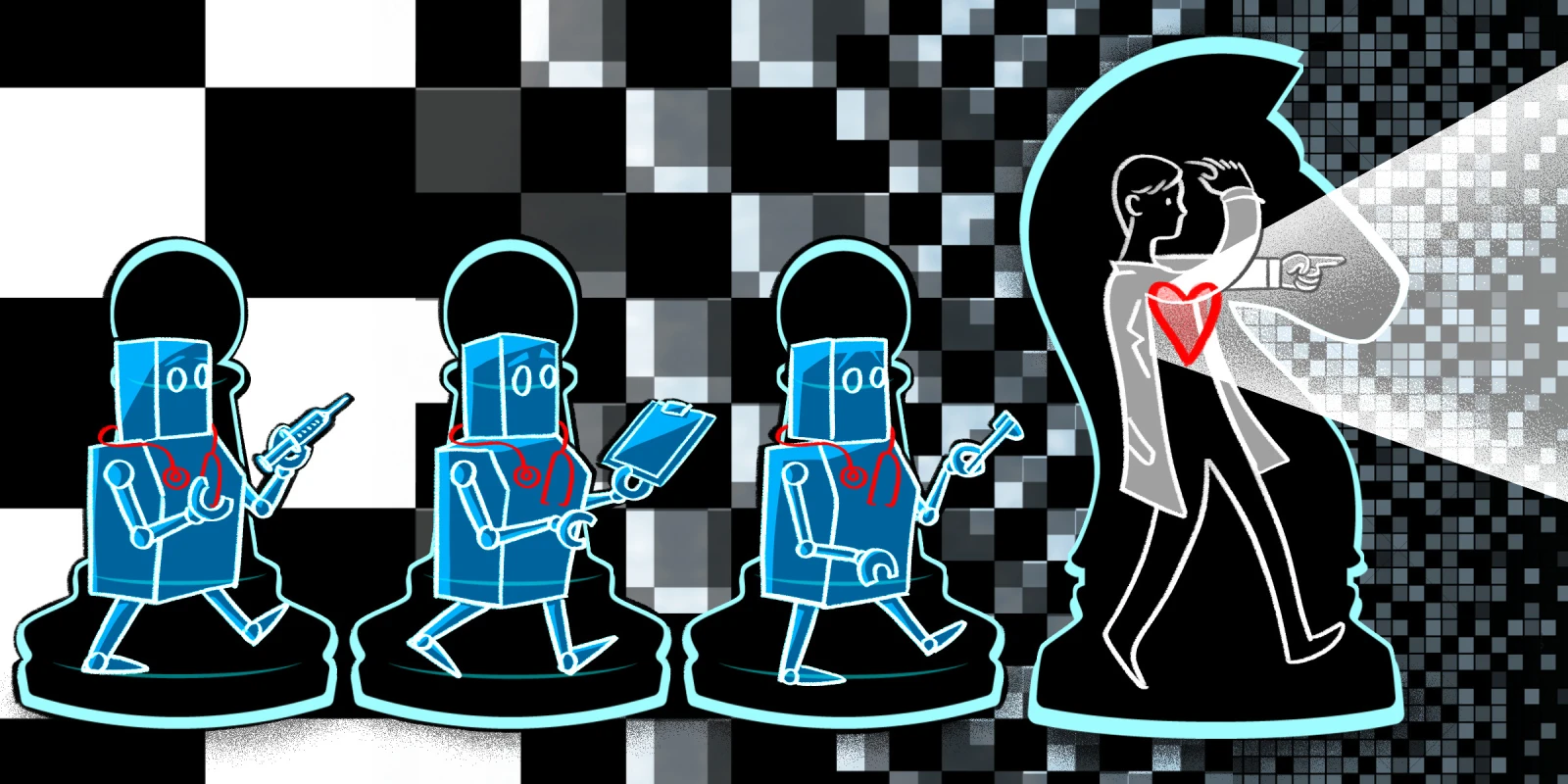
AI has already begun invading medicine. The number of papers, models, and datasets that have been tested in the past year has skyrocketed including discussions in radiology (1, 2), cancer, and cardiology (1, 2, 3, 4). At the pace that these models are being added to and improved upon, it is no wonder that physicians like myself see themselves soon being replaced by a machine. Some crazy theories seem right out of an episode of “The Jetsons”: that physician clinical offices will soon be replaced by massive server rooms, or that patients will enter an exam room full of cameras and equipment, which will examine them, record measurements, and solicit questions to accurately diagnose and treat them.
However, I don’t believe this is the future.
First, we need to understand what tasks computers are good at. As mentioned before, AI systems are fantastic at competing with human players in virtual video games because in these environments, there are specific sets of rules that govern movement and success. Therefore, once you have a fundamental understanding of the governing rules, it is possible to predict outcomes in almost any scenario. Commonly, AI systems run simulations within an artificial environment to create mountains of data to train the system to quantify and explore all possible situations. Once the AI system no longer has to account for added data, the training is complete, and the testing can begin. Video game environments are well-suited for computers because the rules are literally written in computer code and cannot be violated: it’s a well-defined parameter space of specific outcomes.
As we all know, human health is not a well-defined parameter space. In fact, nothing about human health is constrained. For every hard and fast physiological “rule,” there is an “exception” or a case that “defied the odds.” There is no specific set of guidelines or patterns that all human health, physiology, or pathophysiology must follow. There is an absolutely insane number of relevant variables in each situation, which are difficult to parameterize and input as data to a computer. However, for humans, obtaining and interpreting that data is much simpler. Most health care workers can walk into a room and almost immediately tell that someone is sick or in pain. For a computer, this is an arduous task. A computer needs to understand a massive amount of data, including breathing rate, facial expression, muscle tone, skin texture, presence of sweat, smell, and more, just to even begin to decipher if a patient is sick. It then has to determine whether or not the patient is ill or if the patient just finished exercising. Simply put, computers are not good at solving these types of unrestricted and open-ended problems.
Therefore, what medical problems are computers good at? Confined, clear, and well-defined clinical problems, including routine imaging, ECGs, and laboratory values. The stream of data into the AI system is constant: either pixels of images, lines on a graph, or discrete lab values. In an ECG context, AIs already extract important characteristics such as heart rate and key intervals. In imaging, AIs can count ribs, identify missing components, or other routine tasks with very high fidelity and accuracy. Here, the machines perform tasks that are simple “checklist” components that all health care providers are supposed to perform with every study. However, many times, humans neglect these checklists in the heat of complicated cases, preliminary bias, etc., and miss important findings that may be unrelated to the initial clinical presentation but important for the patient’s health. In this example, computers excel at identifying these routine structures and can quickly check for simple abnormalities.
But do these checklist tasks actually improve care for patients? Let’s return to our video game example. In several large-scale video game competitions, AI systems beat humans almost every time. However, when you change the teams, something interesting happens. If you pair a video game “expert” with an AI to compete against other AIs, the human/computer pair wins almost every time.
Why is that? What is happening in this partnership that enables humans to succeed against a system trained to be better than humans themselves? Because humans are far better at strategy. Here, strategy is defined as not always taking the best option at the moment, leading to a better option in the future. Computers and AI systems are excellent at predicting success several or even hundreds of moves in advance, but sometimes you need to “lose a battle to win the war.” With the computer/human pair, humans are freed from remembering and predicting all of the system’s technical innerworkings. They are then free to think about more complex strategic ideas and abstract relationships that will drive future success. Quite frankly, I believe this is why most of us enjoy the medical profession: to critically think, interact with patients, and synthesize data to help patients achieve their health goals. Removing the litany of mundane and simple tasks would enable physicians to develop better relationships with patients and do what they love to do.
In the room with the engineers demonstrating their amazing work, I found excitement overtaking my fear of replacement. Excitement that in the future I would have a partner who expertly counted ribs, determined heart rate and ECG intervals, or identified tracheal deviation. All without a single complaint and asking for nothing more than a power cord.
What are your thoughts about AI in health care? Share your predictions in the comments.
Brian Zenger has a BS in Biomedical Engineering and is a MD/PhD student in Biomedical Engineering at the University of Utah. In addition to his clinical and research responsibilities he is the founding volunteer coordinator and current director of the No One Dies Alone program at the University of Utah. He is an active member of the community serving as a volunteer and in multiple leadership positions. He is a 2020–2021 Doximity Op-Med Fellow.
Illustration by April Brust