Banu Aygun, MD, presented long-term follow-up data from the Realizing Effectiveness Across Continents with Hydroxyurea (REACH) trial at the plenary session. The phase 1/2, open-label, REACH is the largest trial to test hydroxyurea in children worldwide, and among the first to test its feasibility in real-world settings in Africa. Primary study results she presented at the 2018 ASH plenary session showed the study was feasible for enrollment, retention, and adherence.
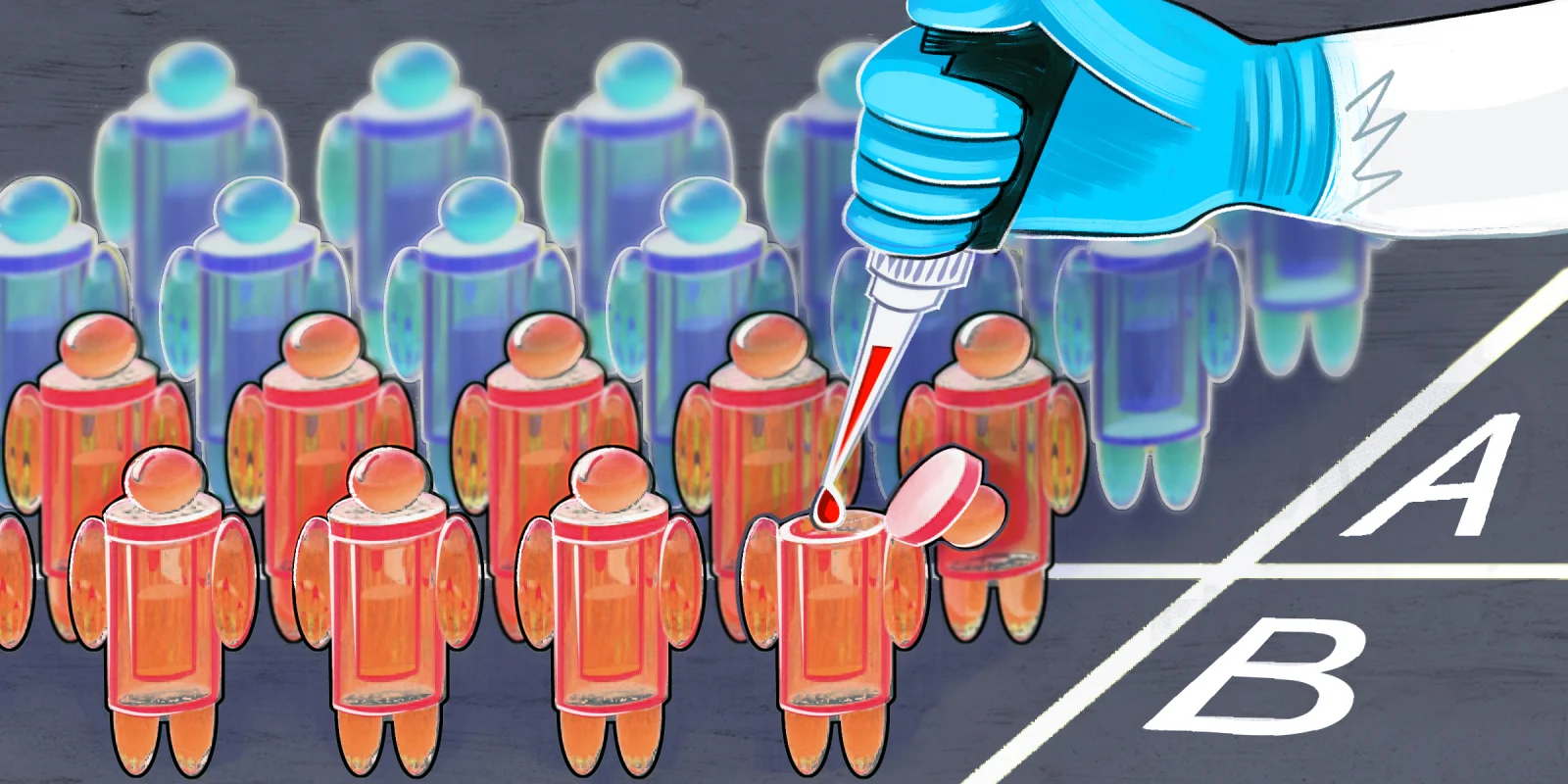
The trial enrolled 606 children age 1-10 years in four sites led by local investigators: Angola, Democratic Republic of Congo, Kenya, and Uganda. The study included a fixed dose safety phase of 15-20 mg/kg/day of hydroxyurea (0-6 months), dose escalation to maximum tolerated dose (MTD; 7-24 months) increasing to 20-30 mg/kg/day, and 24 months of MTD/dose optimization based on weight and laboratory results. The final dose range was 25-29 mg/kg/day, similar to that used in the U.S.
Current study objectives included effects on laboratory parameters and clinical outcomes over time, comparison of hydroxyurea dosing phases, and whether dose escalation to MTD was better than a low fixed dose. Trial participants were age 5.4±2.4 years, a “unique very young patient population;” 86% remain on trial. Average treatment duration was about seven years. There were 44 deaths; the 40 study exits were mostly patient relocations.
Hemoglobin (Hg), HgF, and mean corpuscular volume increased on study drug, while absolute neutrophil count decreased. HgF was persistently expressed at levels >20% during the dose escalation and optimization phases. The incidence of vaso-occlusive painful crises, stroke, transfusions, and serious adverse events decreased during the study. These benefits were seen even during the initial fixed-dose portion of the trial although higher doses were more effective. Safety in the presence of other potentially confounding health risks, like malnutrition and malaria, was also demonstrated. Dose-related toxicities were low.
This trial provides evidence that extended hydroxyurea treatment is safe, well-tolerated, and effective for children with sickle cell anemia living in sub-Saharan Africa. Hydroxyurea dose escalation to MTD, followed by dose optimization, leads to better clinical outcomes without increased toxicities. Sarah O’Brien, MD, press briefing moderator, called this study life-changing for people living with sickle cell disease.
Dr. Aygun said treatment with hydroxyurea at optimal dosing should be incorporated into newborn screening programs that are being developed. “We know for newborn screening programs, it’s not enough to diagnose a condition if you can’t tie it to a treatment. If we are diagnosing children with sickle cell anemia, we have to be able to offer hydroxyurea to them.”
Oliver Shastri reported on a study using artificial intelligence to analyze public social media posts by patients living with sickle cell disease (93% of 513 posts) and caregivers (7% of posts) in the UK. These unfiltered comments outside clinical settings revealed evidence of broad health inequities, including limited access to emergency care and treatment, racial bias, and negative preconceptions when seeking medical care, such as dismissal of pain crises. The group are planning to develop targeted educational programs to improve awareness among front-line health care professionals to address these significant unmet needs.
Dr. Lederman has no conflicts of interest to report.
Illustration by April Brust