Kimmie Ng, MD, addressed the growing problem of early-onset gastrointestinal cancers in her keynote address at the ASCO GI Cancers Symposium.
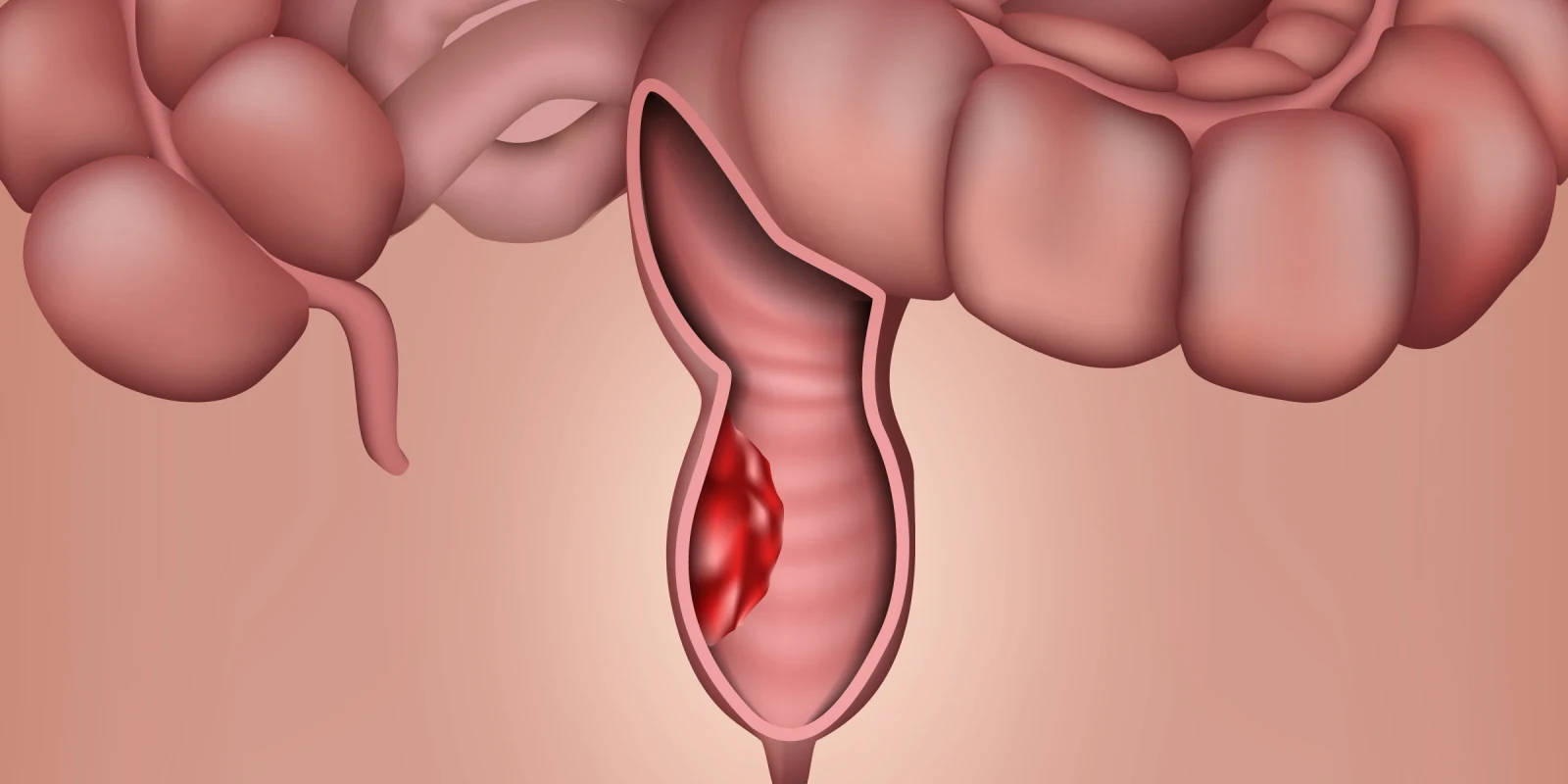
Screening has contributed to the declining incidence of colorectal cancer (CRC) in older individuals. However, CRC incidence has increased by 2% per year in those aged <50 years since the mid-1990s, particularly in non-Hispanic whites, and especially for rectal cancer. CRC is the leading cause of death in young men and the second leading cause of death in young women after breast cancer.
Delayed diagnosis of young-onset CRC is attributable to a lack of awareness among both patients and providers. Younger individuals are more likely to be diagnosed with advanced-stage disease. Although young-onset CRC is associated with a greater prevalence of pathogenic germline variants, most young-onset CRC is sporadic.
Increasing young-onset CRC reflects a birth cohort effect, suggesting modifiable risk factors such as environmental exposure and diet/lifestyle. The Nurses’ Health Study II cohort has identified obesity, ≥40 kg weight gain since age 18, sugar-sweetened beverage consumption, particularly in adolescence, sedentary lifestyle, and being breastfed as risk factors, and adequate vitamin D intake as protective. However, most patients are not obese and follow a healthy lifestyle. Some studies suggest that young-onset CRC may be genomically and epigenetically distinct and associated with a unique microbiome.
Younger patients receive more chemotherapy, surgery, and radiation, even when not indicated by guidelines, and even though more treatment does not produce better survival. The recently published first international consensus guidelines on the treatment of young-onset CRC point out that management should not be age-specific. However, young patients face unique challenges requiring specialized care, as they often experience anxiety or depression, financial difficulties, and are caring for children and/or parents. Dr. Ng highlighted inclusion of recommendations for multigene panel testing and fertility preservation referrals in the guidelines, as the latter often is not discussed during diagnosis or treatment. She noted that young-onset non-CRC (pancreatic and esophagogastric) cancers are also increasing, which is not a screening effect as no screening test exists for them.
Dr. Ng is the founding director of the Dana-Farber Cancer Institute’s Young-Onset Colorectal Cancer Center, one of the first centers to provide specialty oncology care for young patients with CRC. The center supports education and awareness programs for patients and clinicians to address the problem of delayed diagnosis.
Dr. Ng recommends specialized care for young adults with CRC, including universal germline testing and genomic profiling to guide targeted therapy, education of the general public and health care community, erasing the stigma of CRC and related symptoms, and promotion of a healthy lifestyle beginning in childhood. Her research call to action includes life-long prospective cohort studies, investigation of environmental exposures, novel screening and early detection modalities, comprehensive collection of clinical specimens, and international cooperation, because the absolute number of patients is small. In the U.S., Count Me In, a patient-partnered, digital social media platform, is accelerating accrual and biospecimen collection, enhancing racial, ethnic, socioeconomic, and geographic diversity, and enabling research to continue during pandemics.
Dr. Lederman has no conflicts of interest to report.
Image by medicalstocks / Shutterstock