This year’s ACTRIMS meeting was a hybrid in-person and virtual event in West Palm Beach, Florida, from February 24–26. The three-day conference included educational symposia, scientific presentations, and poster sessions with speakers from around the globe. The topics presented included the latest update about previously approved multiple sclerosis therapies and disease-modifying therapies currently under investigation. A major focus was on biomarkers in multiple sclerosis (MS).
While the field of disease-modifying therapy in MS has dramatically expanded in number and diversity of therapeutic options over 20 years, the field has been critically lacking in clinically meaningful biomarkers. Patients are initiated on therapy without the ability to quantify a therapeutic response. A lack of benefit is only identified when a patient experiences breakthrough disease activity. Developing biomarkers for prognosticating or quantifying therapeutic response was a hot topic at ACTRIMS and the subject of many presentations and posters. The biomarkers discussed included blood-based tests and imaging technologies. Unique MRI protocols, optical coherence tomography measures, and seven Tesla-based MRI investigations were among the imaging technologies used to better understand MS. Yet, blood-based measures of disease activity were presented by a wide variety of speakers.
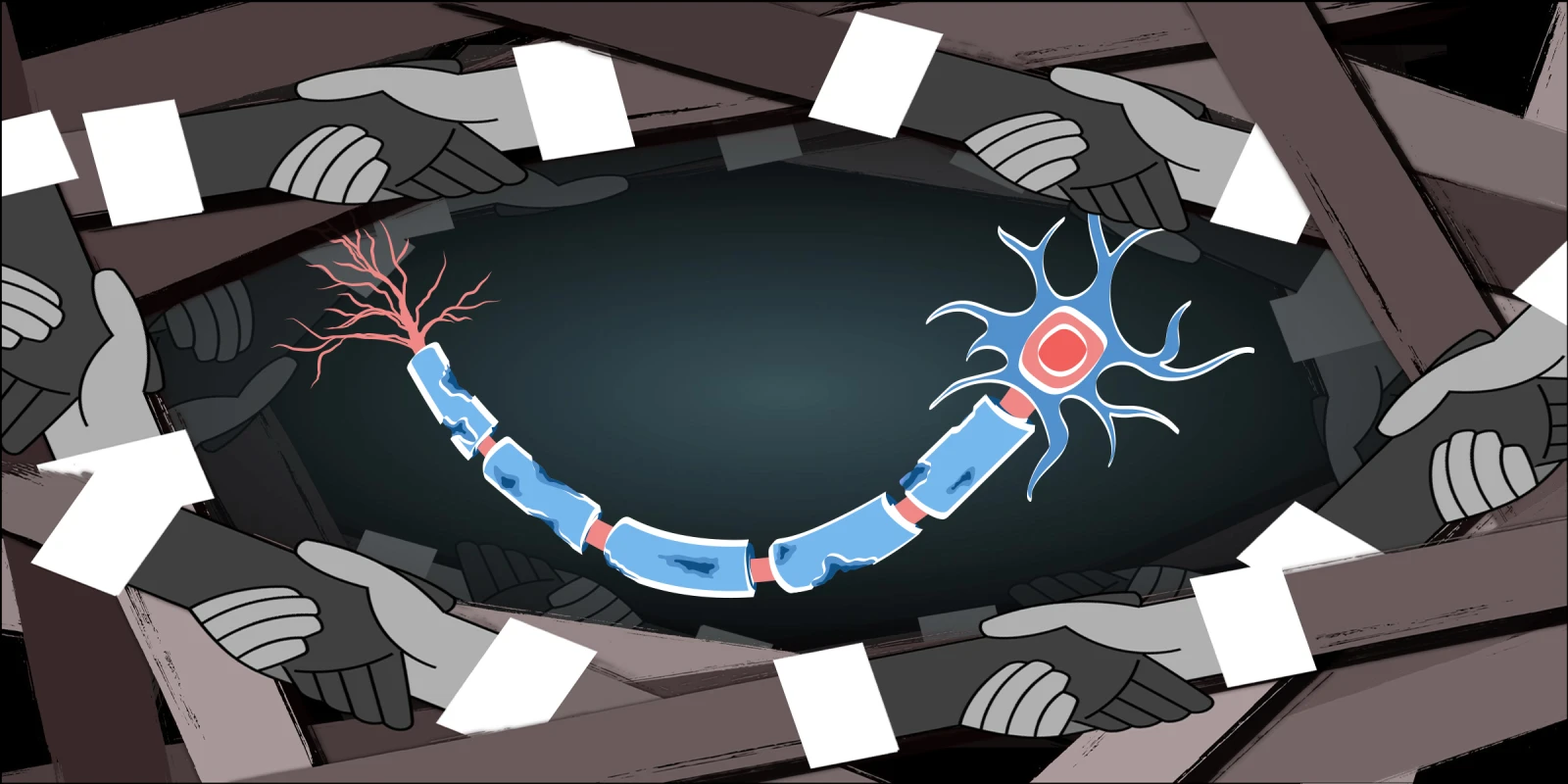
One poster, in particular, stood out to me. The first and last authors were Peter Kosa and Bibiana Bielekova, from the National Institutes of Health. The poster was entitled, “Superiority of serum NFL in predicting multiple sclerosis severity.” Neurofilament light chain (NFL) has received significant attention as a potential biomarker for MS because it is an intra-neuronal antigen that is released into the cerebrospinal fluid (CSF) after damage. Multiple studies have identified CSF and serum NFL as a marker that correlates with damage in MS. Yet, their utility was limited by the variability across patients, based on a patient’s age, weight, and metabolic rate. While the CSF levels of NFL would be representative of neuronal damage, it is not practical to sample CSF frequently, thus there is a need to validate serum NFL levels as a clinically meaningful biomarker in MS.
The authors studied NFL levels in 1,138 paired CSF and serum samples from 328 MS patients, 199 non-MS controls, and 44 healthy controls as part of an IRB-approved natural history study at the NIH. Participants had standardized assessment and sample acquisitions over time, and the samples were subjected to NFL assessments. The data was separated into a training dataset and a validation dataset to determine the ability of NFL biomarkers to predict disease progression. The authors controlled for covariates such as volume of distribution (e.g., weight), protein metabolism (e.g., blood urea nitrogen or creatinine), and age. Their study found that adjusted serum NFL (adjusted in a model that accounts for covariates) correlated best with CSF NFL levels. When compared to clinically meaningful MS outcomes, CSF NFL correlated best with contrast-enhancing lesions on MRI, but serum NFL correlated best with measures of disease severity. The authors hypothesized that the sNFL correlation with disease severity was a result of both brain-based damage and, more importantly, spinal cord-based damage that could result in NFL being released from both upper motor neurons and lower motor neurons.
The importance of this study should be recognized on multiple levels. First, the large sample size provides unique power to the study. Second, the well-curated biospecimens provide a level of confidence in generated data. Finally, the study provides critical data for the field on how to implement serum NFL into clinical practice. Any such application may need to account for several covariates, including age, weight, protein metabolism, and regions of MS plaques. While more research is underway to translate serum NFL into a clinically utilized tool, this study was a critical step in that process.
Dr. Greenberg is employed by UT Southwestern Medical Center. He has received grants NIH, Anokion, Clene Nanomedicine, and Regeneron and consulting fees from Alexion, Novartis, EMD Serono, Horizon Therapeutics, Genentech/Roche, Signant, IQVIA, Sandoz, Genzyme, Immunovant and PRIME Education. Additionally, he has received royalties from UpToDate.
Illustration by April Brust