Secukinumab is safer and more effective in treating psoriatic arthritis (PsA) in patients who have demonstrated previous intolerance or failure to TNF-alpha inhibitor (TNFi) therapy, according to new research presented at the American College of Rheumatology Convergence 2025 (LB01-LB18).
Few treatment options exist for patients with PsA who are either TNFi-intolerant or who have previously failed TNFi therapy. The paucity of treatment options for this patient population sets the premise for the AgAIN study (CAIN457FD304; NCT04632927)—the first randomized, double-blind, active-controlled multicenter trial that directly compares ustekinumab (UST) and secukinumab (SEC) efficacy in patients who are either TNFi-resistant or intolerant.
This study followed 119 patients at 28 clinical centers throughout Germany who were randomized to receive SEC (n = 56) or UST (n = 63). The mean age was 53.5 ± 11.0, with 15.1% of patients being more than 65 years of age. The population was overwhelmingly female in both the SEC (n = 69.6%) and UST arms (n = 65.1%). Nearly one-third of patients in the SEC arm weighed more than 100 kg (n = 30.4%), while 22.2% of UST patients fell into the >100 kg category. All patients included in the study had a PsA diagnosis score ≥ 3 as per the CASPAR criteria.
The following characteristics fell among the important CASPAR features: current psoriatic activity (91.1% SEC, 82.5% UST), juxta-articular new bone formation (37.5% SEC, 31.7% UST), and negative rheumatoid factor (100.0% SEC, 96.8% UST). Researchers included only patients with a prior history of TNFi exposure and failure. Most qualifying patients had received adalimumab therapy previously (68.9%). The UST arm had a higher treatment discontinuation rate (25.4% vs. 3.6% SEC), largely due to reduced or loss of efficacy (mean SD of 24.3 ± 2.0 weeks for SEC vs. 21.5 ± 6.8 weeks for UST). While investigators encountered various hurdles, such as recruitment issues, they still managed to complete the study and produce data that provided a descriptive analysis of comparative efficacy and safety.
SEC outperformed UST in qualitative data across the board. SCE exhibited better efficacy in all areas of clinical and patient-reported outcomes (PROs), but it produced safety signals that better aligned with the known safety profile. Researchers observed improved key clinical endpoints and p=PRO as early as Week 2—effects that persisted through the 28th week of evaluation.
HAD-DI response was the primary endpoint and increased continuously in the SEC arm. This value was much greater in the SEC arm, with a response rate of 57.1% (32/56) for SEC compared to 27.% (17/63 pts) for UST at week 28 [OR=3.647, 95% CI: 1.601-8.311; p = 0.002;]. The SEC group also demonstrated better secondary and exploratory qualitative outcomes. While researchers found no new safety signals in the SEC arm, more than three-fourths (76.8%, or n = 43/56) of patients in the SEC experienced treatment-emergent adverse events (TEAEs). The value was slightly higher in the UST arm, with 81.0% of patients experiencing TEAEs. More patients in the SEC arm experience serious adverse events (8.9%; sec; 5/56 pts) than in the UST arm (3.2%; UST; 2/63 pts). TEAEs accounted for 3.6% of the discontinuations in the SEC arm versus 12.7% in the UST arm (8/63 pts).
Overall, the study’s results show that SEC can help expand the treatment options available to TNFi-experienced patients.
Frieda Wiley, PharmD has no conflicts of interest to report.
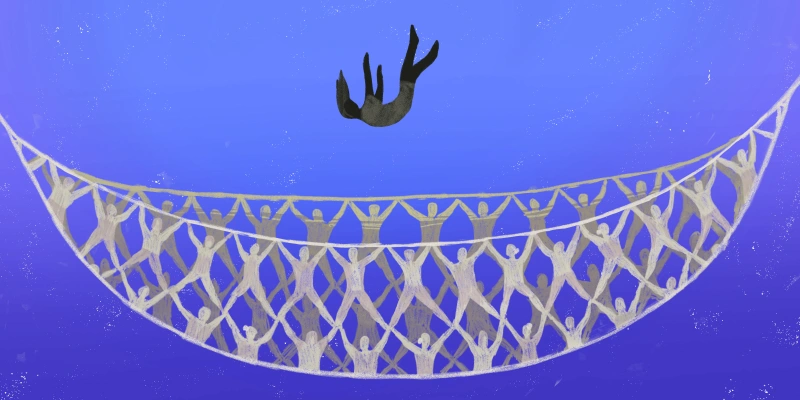
Illustration by Jennifer Bogartz