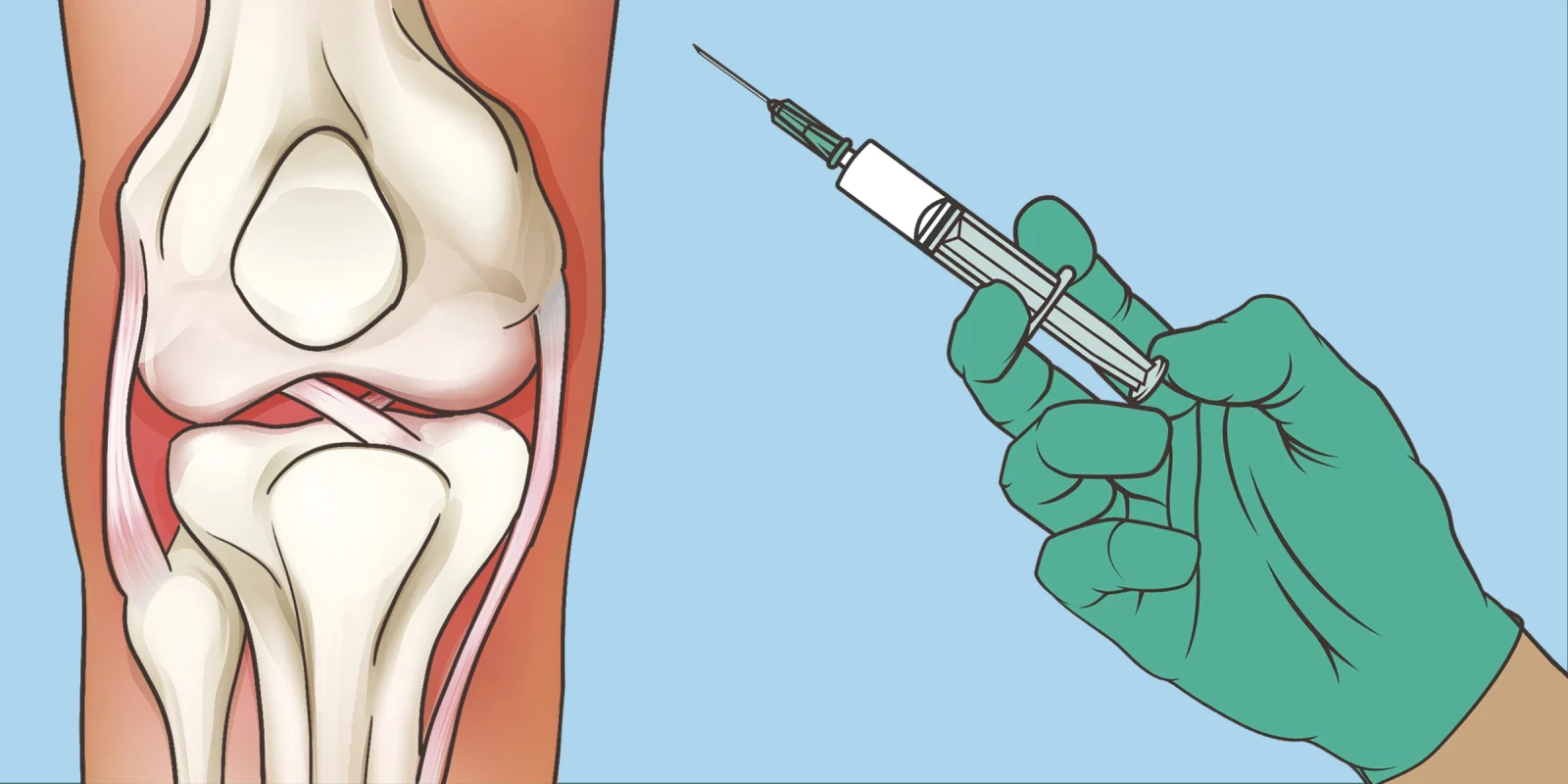
Hyaluronic acid may offer dose-dependent improvements in patients with refractory knee osteoarthritis (KOA), according to a recent study presented at the American College of Rheumatology Convergence 2025 (Abstract No. LB07, Adipose-Tissue Derived Mesenchymal stem Cells vs. Hyaluronic Acid in Refractory Knee Osteoarthritis in a low-resource setting: A Phase IIb RCT).
A leading cause of disability, no disease-modifying therapies currently exist for KOA. While hyaluronic acid (HA) has remained a longstanding staple in KOA treatment, there is a paucity of head-to-head data comparing the HA to adipose-derived mesenchymal stem cells (AdMSC) therapy. This study evaluated the safety, efficacy, and dose of response of AdMSC versus HA of intermediate weight in Bengali patients with refractory primary KOA.
This evaluator-blinded Phase IIb randomized controlled trial included 73 participants with a Kellgren-Lawrence grade ≧ 2KOA based on standard conservative care. A randomized selection of these patients received HA injection (n =31), a single dose of AdMSC injection (n = 21) or two-dose AdMSC injections (n=21, dose interval 3 months). A multidisciplinary team evaluated the primary outcomes, which included knee-related problems on KOOS, pain on CAS, femoral cartilage thickness assessed by ultrasound, and MRI-assessed cartilage defects at 0, 6, and 12 months.
At baseline, all patients averaged 60 years of age across the three groups (60.8 ± 8.14 years in the active control HA group; 60.76 ± 6.69 in the single-dose AdMSC group; and 58.10 ± 5.67 in the two-dose AdMSC group).
All patients were either obese or borderline obese, with body mass indexes ranging from 26.12±2.73 in the active control HA group up to 27.65 ±2.76 in the single-dose AdMSC group. More patients in the HA group had comorbidities than any other group, and 19 (61.29%) of the 31 patients in the HA group fell into this category. The single-dose AdMSC group had the fewest comorbidities, with slightly more than half (n=11 [52.38]) of the 21 patients in this group having another health condition.
Patients experienced dose-dependent improvements in both quantitative and qualitative outcomes, as noted by the interim analysis. In addition to greater pain reduction (3.2 vs. 1.3 points), those who received two doses of AdMSC showed greater overall functional improvement (21.24 vs. 11.31 points) compared to HA at 6 months (p < 0.001). Cartilage increased by 0.25 ± 0.18mm in thickness, while two-dose AdMSC administration improved defects by 9.113%. Cartilage deterioration occurred in the HA group (0.06 ± 0.14mm; 0.75). Patients who received single-dose AdMSC therapy also had better outcomes than those in the HA arm. Investigators did not identify any baseline predictors, and patients tolerated all treatments well.
This study’s results indicate that two-dose AdMSC therapy produced significantly better outcomes in pain symptomatology, cartilage structure, and function. The findings provide additional evidence supporting the need to expand to Phase III clinical trials with larger patient populations, focusing on South Asian where KOA continues growing in prevalence.
Frieda Wiley, PharmD has no conflicts of interest to report.
Collage by Diana Connolly / Shutterstock