Before I ever dreamed of becoming a doctor, I knew I wanted a career that would allow me to take care of my parents. Watching them care for their own parents — balancing work, family, and cross-continental responsibilities — instilled in me a sense of duty to one day do the same. When my grandfather began showing signs of dementia, my mother, despite having a full life in the U.S., made frequent trips back to China to support him. She did everything she could to be present, both emotionally and financially. Witnessing that devotion taught me that aging inevitably leads to a reversal of roles, where the child becomes the caretaker.
As I pursued academics and prepared for my future, this responsibility remained abstract — something distant and inevitable, but not yet real. That changed during my inpatient rotation on general neurology.
I met a patient who was 53 — exactly my mother's age. He had a history of frontal lobe glioblastoma multiforme, status post resection, and was undergoing treatment with temozolomide, radiation therapy, and Avastin. He came to the ED after an infusion, presenting with increased tremors, behavioral changes, and confusion. I was on call that night and got to know his medical history and the personal side of his life.
What struck me most was his support system: his children. His eldest son — younger than I am — was his primary caregiver. Through the chart and MyChart messages, I saw a young man diligently coordinating treatments, communicating with the care team, and now bringing his father to the ED. Most people his age are preoccupied with finals or adjusting to post-grad life. He was managing chemotherapy schedules and monitoring his dad for worsening symptoms of brain cancer.
This patient was admitted to the service I was on that week, so I saw him during morning rounds. His workup was unremarkable — no infection, no acute tumor progression — so we planned for discharge with PT, OT, and close neuro-oncology follow up. The question of whether to send him home or to a care facility sparked discussion. He needed 24-hour supervision, but his sons had arranged their schedules to ensure that one of them was always home with him. Ultimately, he went home, supported by a family deeply committed to his care.
Though I didn’t meet all his sons, I could see how much he trusted and appreciated them. Their relationship, likely reshaped by illness, demonstrated a kind of strength and devotion that left a lasting impression on me. I wondered how their bond had changed and how they were managing the emotional and practical toll of caregiving.
This experience prompted me to think more deeply about my parents — and how I have been privileged to pursue my education and training without needing to worry about them. My mother has often told me, “The greatest gift I can give you is my health.” While I have always insisted that I would take care of her no matter what, I now have a deeper understanding of what she meant. Health, for both patients and their families, is a gift that offers freedom — not just from illness, but from the weight of constant vigilance and responsibility.
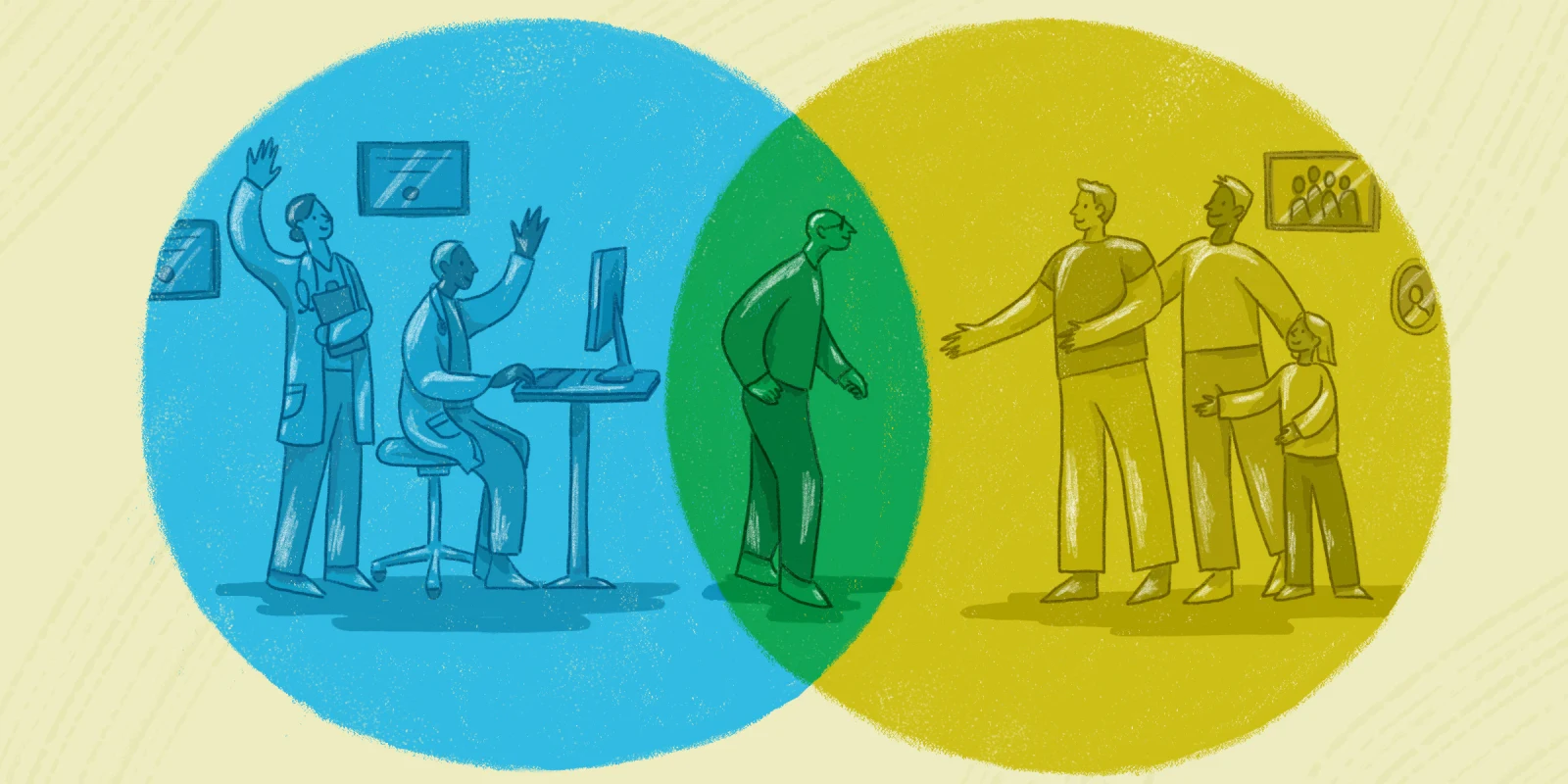
This experience has broadened how I see my role as a future physician. Beyond treating disease, I will care for people embedded in families, communities, and complex relationships. I’ve come to appreciate how essential caregivers are — not only for the practical aspects of care but for the emotional well-being of patients. Every clinical decision, from discharge planning to medication timing, affects them, too. Recognizing this will shape how I communicate, how I advocate, and how I make patient-centered plans.
More than anything, this patient — and his family — taught me that medicine is not practiced in isolation. It happens in homes, in late-night phone calls, in sons driving their fathers to appointments. Their story serves as a constant reminder to me, as a soon-to-be resident physician, that to truly care for a patient, we must also see and support those who stand beside them.
How has your relationship with the caregivers of patients impacted your practice of medicine? Share in the comments.
Patient name and identifying details have been modified to protect privacy.
Malinda Gong is a fourth-year medical student at the University of Virginia in Charlottesville, Virginia. She will be applying to diagnostic radiology this year and has a special interest in breast radiology. She enjoys spending time with her two dogs (Stanley and Piper), baking excessively, and completing paint-by-numbers projects in record speed.
Illustration by Diana Connolly