Victor Ekuta is a 2020–2021 Doximity Research Review Fellow. Nothing in this article is intended nor implied to constitute professional medical advice or endorsement. The views expressed in this article are those of the author and do not necessarily reflect the views/position of Doximity.
Sex, gender, and race bias in evaluating and assessing cardiovascular disease are well-documented. In a recent study, Breathett et al. provide additional evidence that women, especially African American women, experience more bias concerning their physical appearance, social support, and prior care as compared to men in the decision-making process for allocating advanced heart disease therapies, such as heart transplants and ventricular assist devices (VADs).
While the results are provocative and consistent with previous literature, the study has notable weaknesses, all of which are acknowledged by the authors. The study highlights a clear association between race, gender, and clinical decision-making, but lingering questions remain. For example, bias was present in participants from both majority and minority groups, potentially suggesting pervasive clinician bias that may reflect internalized aspects of clinical training. Given the widespread use of race-based medical vignettes in clinical training, additional studies should explore this possibility. Additional research is also needed to understand why gender and race were not associated with the allocation of advanced heart failure therapies as hypothesized, despite evidence of bias. Lastly, it remains unclear why the final recommendations made for allocation of advanced therapies favored VADs over transplants.
Overall, the study raises significant concerns regarding the effect of bias on clinical decision-making and highlights the need for improvements in access to advanced heart failure therapies for women and patients from minority groups, as well as the need for interventions to decrease health disparities in the assessment process. Though many clinicians have altruistic plans for their patients, this study suggests that many of us may be susceptible to race and gender biases, which may render our clinical decision-making inequitable. We owe it to our patients and ourselves to identify and address these biases to create a more equitable medical system. As a burgeoning trainee, I plan to do just that.
Victor Ekuta is an MD candidate at UC San Diego School of Medicine. He has previously served as a TEDMED Research Scholar and a Doris Duke Clinical Research Fellow, among many others. In the future, he plans to specialize in academic neurology as a physician-scientist-advocate, employing novel approaches to treat human brain disease, combat health disparities, and boost diversity in STEM.
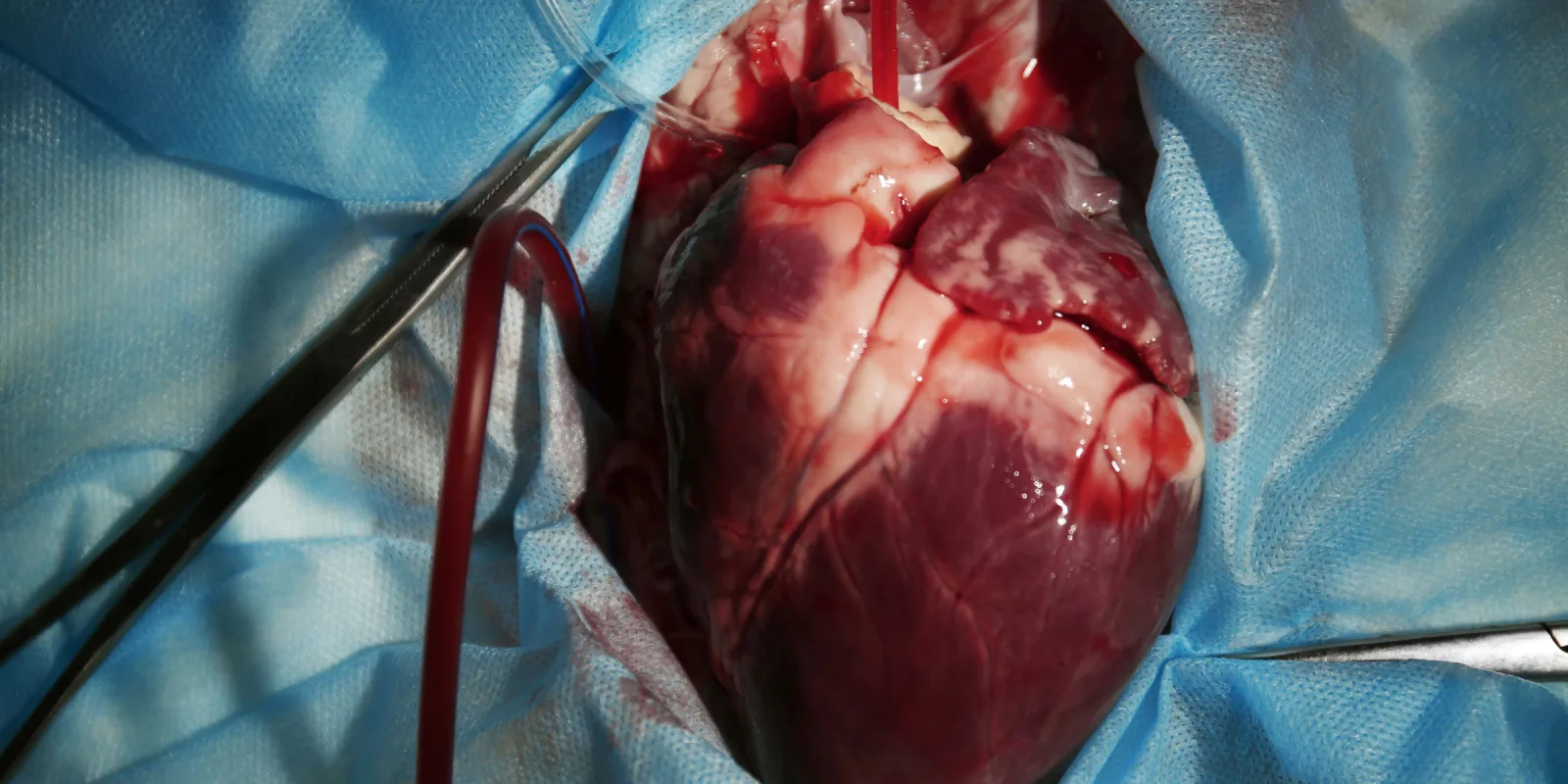
Image: africa studio / shutterstock