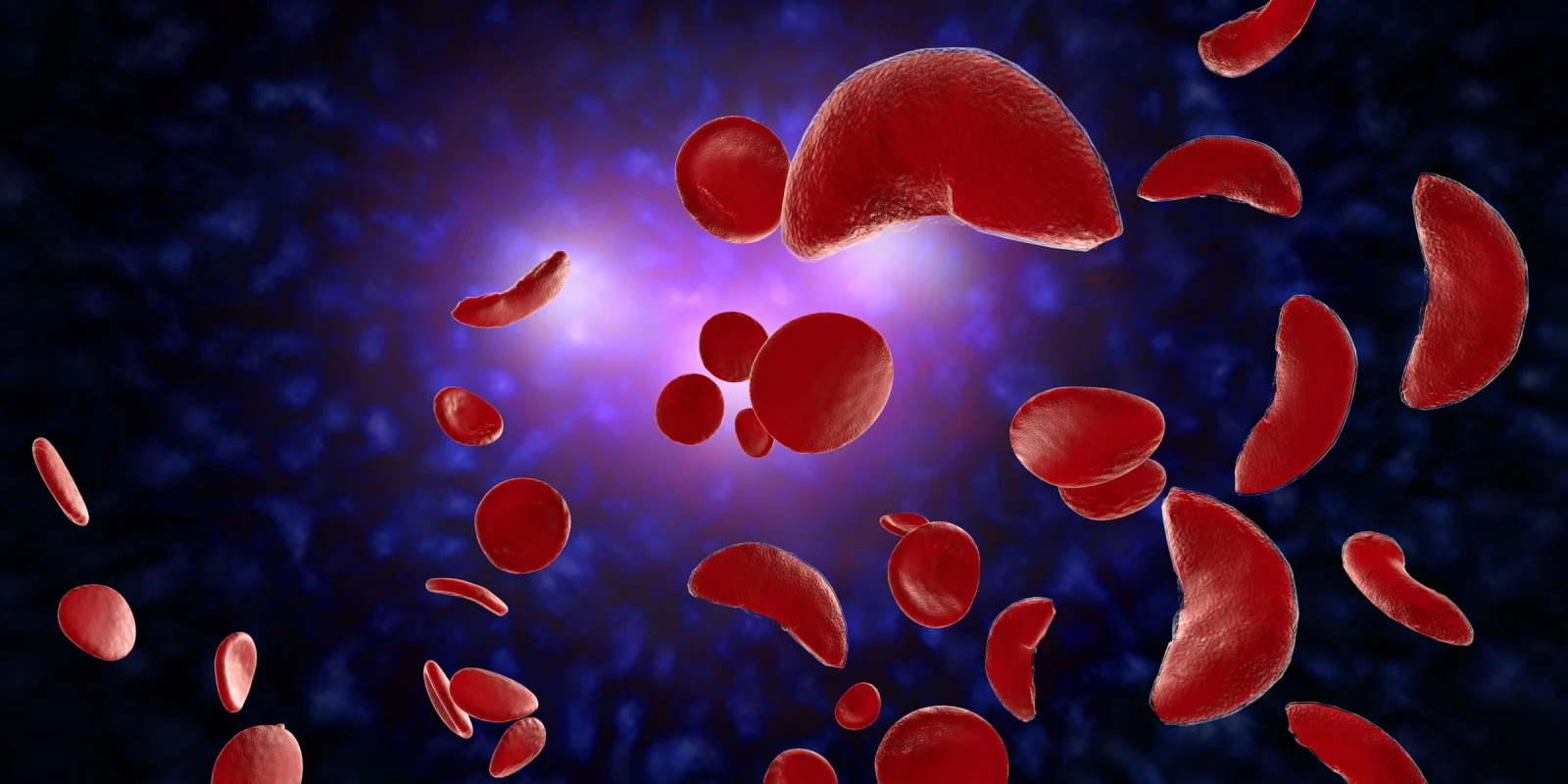
I once had a colleague ask me: What is the least satisfying disease to treat? I thought of a few potential answers but before I could answer, he said it was sickle cell disease. I had to think about this for a moment but in many regards, he was correct. Being a lifelong disease that begins to manifest in peoples' youth and is associated with horrific complications including chronic pain, avascular necrosis, pulmonary hypertension with limited treatment options available, there are few diseases that are both more difficult to treat and have less satisfying options. Within the last several years, a handful of options had become available. But now, many of these options are no longer available. Leading me to ask the question … now what?
Sickle cell disease (SCD) remains a significant public health challenge in the U.S., affecting approximately 100,000 individuals. Despite advancements in understanding the disease, treatment options remain limited, and many sickle cell warriors experience suboptimal management. In recent news, a commonly used option has been withdrawn from the market abruptly, further limiting the options available for this disease.
Current Therapeutic Options and Challenges
The treatment landscape for SCD has seen limited progress, particularly concerning disease-modifying therapies. Hydroxyurea remains the cornerstone of management; however, patient adherence is low. Many patients report inadequate efficacy or side effects, such as alopecia, nausea, and nail bed changes leading to discontinuation. However, we have found that in practice, many patients are poorly informed on the actual benefits of hydroxyurea. Beyond potential benefits in limiting pain crisis, potential benefits include organ protection and likely extension of survival. Sickle cell warriors often don’t understand that hydroxyurea can help to limit or delay some of the kidney or lung damage that are hallmarks of end stage SCD. Therefore, I often counsel patients that even if they don’t immediately notice a benefit in pain reduction, the hydroxyurea can still have a major impact in their life. In my clinical experience, fewer than 30% of newly diagnosed adults are on hydroxyurea, and even with continued education and support, this number rises only to approximately 50%. Opinions are often strong and increasing education important.
Recent developments, such as voxelotor and crizanlizumab, raised hopes for improved outcomes. Unfortunately, voxelotor has been withdrawn from the market due to unfavorable results in non-U.S. trials, and crizanlizumab's confirmatory studies failed to replicate initial benefits. These setbacks have left the field with more questions than answers and are removing options some patients relied upon. The patient perception to removal of these agents has included disappointment, shock, and has increased the lack of trust that already existed. Crizanlizumab had initially shown improvement in hospitalization rates for SCD. The hospitalizations often lead to missed days of school, work, relationships, etc. Depression rates are often higher when hospitalizations go up. When data emerged questioning the benefits, many patients opted to discontinue crizanlizumab despite it still being available in the U.S. Many of these patients seemed to be benefiting but negative data and concerns led them to stop. Voxelotor had been an encouraging therapy that showed elevation in hemoglobin levels. Being able to show patients trends of hemoglobin levels improving offered patients a sense of comfort that this agent was working. The benefits of several agents were harder to show objective proof for. Elevating hemoglobin levels offered that objective proof. Voxelotor now being removed gets rid of a safety net that many patients relied on.
L-glutamine has been better received among patients, likely due to its perception as a dietary supplement rather than a pharmaceutical agent. While it may provide some benefit by strengthening red blood cells, it is not designed to modify the underlying pathology of SCD. I believe one of the reasons L-glutamine has been somewhat more accepted is I often present it as a supplement at its heart and a supplement known to increase muscle mass. Treating SCD and increasing gym gains is attractive to many.
Emerging therapies, such as casimersen and other gene therapies, offer potential but come with high costs and logistical challenges, limiting access for most patients. While this therapy has the potential to modify the disease with a one time therapeutic option, the lack of long-term data, the cost, the need for chemotherapy, and the thoughts of editing genes make many hesitate.
Systemic Challenges in Care Delivery
SCD patients frequently utilize health care resources, leading to increased lengths of stay and ER visits. The lack of disease modifying therapies limit our abilities to manage this disease away from acute care settings. Efforts to reduce hospital admissions have not translated into enhanced outpatient support. Many centers lack the infrastructure for urgent outpatient interventions, such as IV fluids and pain management. The absence of dedicated care teams, transition plans for pediatric patients, and comprehensive psychosocial support further complicates the management of SCD. It is unfortunate that such a large gap exists for this population. Other less common conditions, such as cystic fibrosis, have had more research dollars and more dedicated centers available to increase access of care compared to SCD. The limited investment has delayed important advancement.
Research Gaps and Clinical Trials
The design of clinical trials in SCD presents unique challenges. Subjective endpoints, such as reductions in hospital utilization, may not accurately reflect therapeutic efficacy. Additionally, the historical mistrust of clinical research that has emerged from abuse including the Tuskegee trial, particularly within minority populations, hinders recruitment and participation. Rigid trial protocols often exclude patients who cannot meet stringent criteria, limiting our understanding of treatment effects in diverse populations.
Adverse events reported in clinical trials often reflect the underlying disease rather than the therapies themselves. For instance, while recent concerns regarding voxelotor's impact on crisis frequency have emerged, it is essential to contextualize these findings within the natural history of SCD. Often we are reporting adverse events of disease rather than the therapy.
The current state of SCD management highlights significant gaps in treatment and care delivery. A multifaceted approach that includes improved patient education, enhanced outpatient resources, and inclusive clinical research is essential to advance care for this underserved population. As we navigate these challenges, the question remains: How can we best support individuals living with SCD to improve their quality of life and health outcomes? Or in other words, now that we have lost another one of the few options available to us … now what?
Dr. Landau is the medical director of hematology telehealth for the Medical University of South Carolina. He has served many roles throughout his career at different organizations including Chief and interim Chair.
Image by Ezume Images / Shutterstock