We are always trying to communicate more effectively in the physician-patient relationship because so much of the success of our encounters depends on it. The physician-patient relationship encompasses four core ethical principles: autonomy, beneficence, nonmaleficence, and justice. The onus is on us to provide enough information and guidance for competent patients to make their own decisions regarding the treatment they choose to receive or decline. Our patients have autonomy, the right to accept or decline offered care, and physicians have a duty to respect their decisions.
Of course, these lofty ideals are a lot easier said than done. Physicians frequently face challenges in broaching “difficult” topics with patients and their families. What makes any circumstance difficult is the way we perceive it. For example, I find it difficult to run a mile. Yet my friend runs marathons and finds it quite easy. If we could better manage our perception of challenging conversations, we might dread these discussions less and be more likely to achieve the desired goal of informing and persuading others.
Our conversations are complicated by language differences, cultural barriers, and our patients’ wishful thinking about our ability to fix anything. As human doctors communicating with other human patients, we still crave approval. It makes us feel worthy. Approval is a euphoric drug that enables us to think positive thoughts about ourselves and our abilities. Disapproval feels like an existential threat.
Have you ever thought that, if everyone just liked you and believed you were the best doctor ever, then you would be extremely confident and your practice would be much easier? What would your practice of medicine look like if you did things in a way that made all the attending physicians, nurses, and patients like you?
Do you ever notice that, if and when people disapprove of you, you want to avoid them or get defensive or judge and disapprove of them in return? Our brains are good at focusing on how we can get people to like us.
What really makes our conversations with patients or their families difficult are the negative feelings that come up within us when they get mad or disagree with us. Fortunately, other people can’t control our feelings. They have every right to think and feel the way that they choose, but that doesn’t mean we should allow it to control how we feel.
We can offer our patients the best medical advice, but they don’t have to accept it. If we can release the need to control other people and not be offended or get defensive because of their decisions and actions, we can feel better even in the midst of tense exchanges.
Those messy situations at the end of life are not helped by employing euphemisms. To avoid pain for the family and to protect ourselves, physicians often soft sell the end-of-life message: “Your mother is dying” becomes “your mother is failing.” But this could make the family think that, if only mama or the medical team were trying harder, she might do better. Vague messages create confusion, mistrust, and unrealistic expectations among families.
We need to anticipate and accept the family’s sadness, anger, and disappointment. If we are confident in communicating our message and act in the best interest of the patient, we can better accept the family’s negative thoughts and feelings.
How can you set yourself up for success when you need to have a challenging conversation?
You can test whether you should be giving feedback or relating news by examining how you feel. If I’m feeling upset, frustrated, or angry with a patient or a family, I’m probably going to relate information and recommendations in a certain tone that will convey those negative emotions. But if I can clean up my own thoughts and get to a place of compassion, acceptance, and concern for the patient, I can feel good about how I show up, even if the patient or family is upset with me.
In that state, I can tell a distressed family that, though I understand their anguish over the decline of their father, aggressive care and interventions will actually prolong his suffering. I can let the patient and the family be mad at me without being mad at them. I can even tell them that I understand why they might feel that way. I can’t control their feelings because I can’t control their thoughts.
If a family member is frustrated about how a situation unfolded, I highly recommend offering an apology. Apologies can be soothing. You know that you mean you are sorry about their thoughts. Even if the person is confused or wrong about what they think you did, offering an apology is the opposite of being defensive. It opens up communication instead of shutting it down. Many states have disclosure/apology laws designed to protect our communication regarding negative events, including expressions of sympathy or regret, from being used as evidence of malpractice in liability litigation or administrative action.
Lastly, I would suggest that you listen to the other person and consider the possibility that you could be wrong. One way to defuse an argument is to concede defeat by saying, “You could be right.” It’s not our natural response, and it feels terrible to be wrong. Yet it’s important to recognize that someone else’s disapproval or disagreement is not a referendum on your character or expertise. You are still an excellent physician, and you are worthy. You need to have your own back and remember that you are acting with beneficence and compassion for your patients and for yourself. Now summon your courage and go have that conversation!
Have you had a difficult conversation with patients or their family members recently? Share your experience in the comment section below.
Dr. Naidorf is a board-certified emergency physician living in Alexandria, Virginia.
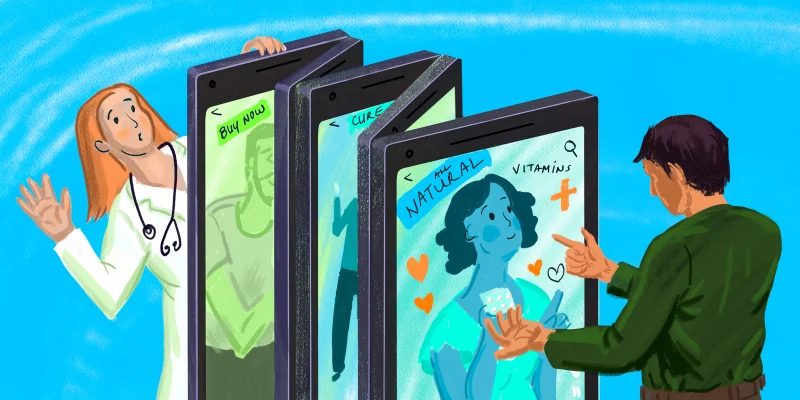
Illustration by April Brust