I hope by sharing my experiences during this transition year from fellow to attending will help others not feel alone. I truly believe that we all have had similar feelings when starting out. There is no shame saying that it is unnerving and we do not know it all. It should not be seen as a shortcoming. I believe that staying transparent and humble it helps us remain connected to those we are caring for.
Below are the top five things I have learned this first year in practice.
1. There is no amount of preparation that can make you ready for the transition.
When I finished my fellowship, I thought that I would be able to handle anything that was thrown my way. I had seen so much during my training, especially as the fellow on call at night. I had seen the sickest patients—taking care of them without someone there to hold my hand. I did not think there was anything that I had not seen—there was nothing that could surprise me. Well not literally, but I at least felt well trained by my program.
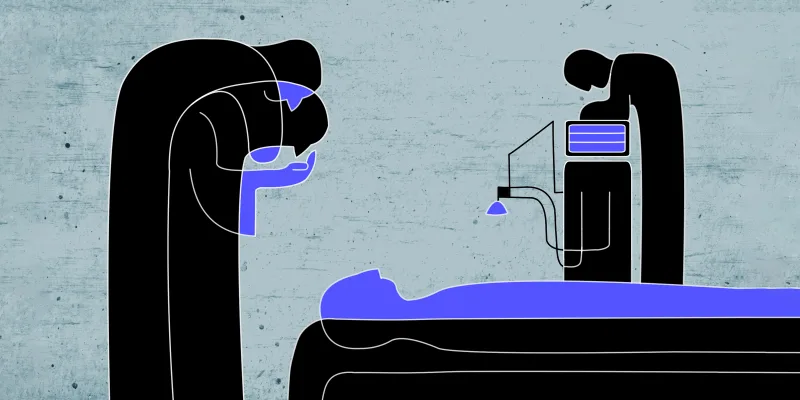
However, I have learned it is quite different to be the fellow stabilizing patients overnight and the attending who is ultimately responsible for the patient. It is not that I am managing conditions that I have not seen, but rather the totality of the decisions I make. There is no one waiting for you to sign out the patient to. Someone to make sure that you have not missed anything. To ensure that you are applying the appropriate guidelines and ordering the corrects tests and interventions. The mental transition has been one of the hardest parts of this year.
2. It is a lot harder than it looks.
This goes back to the first point. You are now required to make decisions that you believe in. You have to trust yourself and believe that you are making the best decision for your patient. This can weigh heavily on you.
There is a mental resilience you have to develop over this first year that no one really talks about. No words can really explain this change in perspective. It may sound strange. You were the one on call by yourself overnight making decisions for very sick patients without the help of your attending, but now it is more than just a night on call. This is someone's life that is being entrusted to you indefinitely. You have colleagues to discuss cases with and the patient is ultimately the final arbitrator, but you are there to guide that person and a great amount of trust is placed in you to do that to the best of your ability.
3. Promotion of a healthy lifestyle means more than you ever imagined.
Once you have accepted the amount of responsibility that has been placed in your hands, you now have to figure out how you want to practice. We all know the rising epidemic of obesity and the impact it has on metabolic abnormalities and cardiovascular disease, but while training, we focus on the complex diseases that require skilled interventions. In fellowship, I was amazed by all the nuances in advanced cardiovascular disease and super specialization in the academic center. There were many patients that came to the university for a second or even third opinion.
Now practicing in the community setting, I have come to appreciate the importance in lifestyle modification. Do not get me wrong. There are still patients with complex disease, but weight loss and exercise have such a great impact on cardiovascular disease that I had known about but never advocated to the extent that I do now. I did not appreciate just how important it is to eat a balanced diet, decrease portion size, increase activity level, and treat sleep apnea. I took for granted counseling on these lifestyle changes and would spend very little time discussing these changes. Even when it came to polysubstance abuse, I would spend only 5 minutes on the subject. My counseling could be summed up as telling the patient to "quit". Now I spend time exploring the relationship to the food or drug addiction. I try to meet the patient where they are and understand how I can help.
4. Be patient. Each day gets a little better.
At first, I was overwhelmed with all that I needed to accomplish in one day, while trying to make the right decisions for my patients. But as each day passes, I feel a little better. I find myself feeling more confident in my decisions and reading more and more about medical management. I take pride in what I do, but understand that I have limitations and that I am not perfect.
5. There is an undeniable connection you feel to your patients.
The most satisfying part of this first year has been how connected I feel to my patients. I care deeply for each and every one of them. I did not realize how much of me I put into everyone I care for. I am not there just to figure out the diagnosis and treatment, but to heal through body, mind, and spirit.
One wise patient told me that we are more than just the sum of our parts and I have no doubt that this is true. I have learned that as busy as things get, the moments when I am truly present with patients are irreplaceable.
Dr. Fola Babatunde is a Cardiology fellow at the Washington University School of Medicine in St. Louis. She graduated from Harvard Medical School and completed her residency at Duke University Medical Center.
Dr. Babatunde is a 2018–19 Doximity Author.