“Is this normal?”
I’ve lost count of how many times I’ve been asked this question. I’ve been bombarded with it since Day One of medical school. This is the question that defines our profession: is this normal? I’ve been asked it by my patients, my professors, my preceptors, my colleagues, my parents, my wife, my attendings, and I’m sure that if my cat could talk, one of the many, many questions she would ask me is, “IS THIS NORMAL?” In her case, I would say, “No, no. A talking cat is not normal.” And I’m fairly certain that I would be right in telling her that.
As for the rest of them, I can’t say that I’ve always answered that question with certainty (though I certainly have tried my best to pretend to). In fact, I’ve found that the further along I’ve progressed in my training, understanding, and practice, the less sure I’ve become of what’s normal. Which I think is great, really. Why is it great? Well, because “normal” isn’t a real thing. “Normal” is a useful concept we have that helps us to define and describe data and phenomena at the population level, large-scale, as a way to understand what is otherwise just that: data. Data is amoral, agnostic, and objective, while normal is a judgment call. That puts physicians in a unique position in regard to answering the question “what is normal?” because as experts and professionals, normal is normal when we say it’s normal.
I’ve heard varying responses from physicians I’ve worked with about this idea, and of course it’s always colored by their choice of specialty. Internal medicine docs tend to say, “That’s not important, what’s important is the trend,” while my pediatrics preceptor might have said, “That’s OK, it’ll probably be normal in a few months.” A surgeon might say, “It’s not usually like that, but it’s not abnormal,” and a pathologist might just shrug and be like, “I’ve seen worse.” With psychiatrists, the answer I seem to get the most is “it depends.” And as a psychiatrist myself, I have to agree with that.
I’m becoming more and more aware of this fact as my training wears on this year. When we’re among our colleagues, we have a shared understanding of what normal is, as is dictated by our education and training, and it’s an incredibly useful tool for diagnosing and summarizing a patient’s situation. Even more so, we learn that there are many layers of “normal” that must be considered as we work towards treatment plans. Patients, of course, have none of this background, none of this training, and, most of all, none of the interest that we had in learning it. They instead rely on us to deal with it, break it down, and make it simple for them. To them, “is this normal?” has only one of two answers.
That makes me ask another question: what does it mean when I answer “yes” or “no”?
This “yes/no” dilemma that I have is rooted in the fact that medicine, psychiatry in particular, has had a complicated history with answering this question of normal with just a simple “yes” or “no.” That’s because medicine isn’t just a powerful discipline in an objective sense, where we learn to understand and manipulate the mechanical, physical, and naturalistic processes of the body in the promotion of healing — it’s also a powerful tool of culture, where those who practice it are granted esteem simply by virtue of the title and whose words carry serious cultural clout. It’s the second part of that concept, though, that really makes me stop and think.
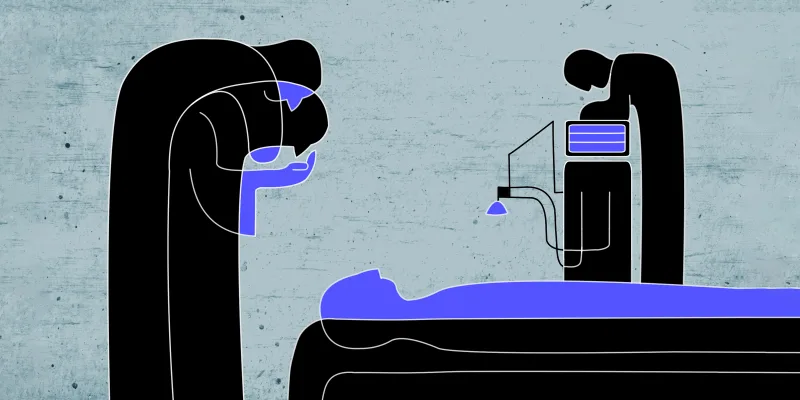
Physicians, like experts in other fields, are gatekeepers of normalcy. However, by virtue of our expertise being tied to such primal cultural ideas like “health” and “fitness,” when we say that something is “normal,” it can often mean so much more. An oncologist telling their patient that “things are back to normal” can mean a new lease on life. An ob/gyn telling an expectant mother who had a worrying quad screen that her baby is “perfectly normal” can be the difference between buying a two-bedroom or three-bedroom house. A psychiatrist telling a patient and their spouse that feelings of guilt, helplessness, and insomnia are “normal” after losing a parent can mean that they don’t have to be anxious, afraid, or ashamed of those feelings. And saying things are “not normal” can be just as powerful.
As gatekeepers, we have the power to open the gate as much as close it. This power is one that many seasoned physicians are familiar with, but as an intern it is still a very new sensation to exercise this power. This is especially obvious in psychiatry because our specialty dabbles in behaviors, thoughts, and beliefs: the building blocks of culture. The history of the practice has, in turn, had its fair share of missteps: the diagnosis of homosexuality as a mental illness; psychosis and schizophrenia being a manifestation of demonic possession; and even promoting the idea that mood disorders or impaired development were purely the result of bad mothering. We’ve done our best as a field to distance ourselves from these statements since then, but they continue to influence how many people think about these ideas, simply because “psychiatry used to say.”
It’s important to me to remember that these beliefs and statements were mostly well-intentioned, but ultimately a product of their time; the stark truth is that society seeks stability, stability requires normalcy, and normalcy is an act of exclusion. There are behaviors, thoughts, and ideas that are destabilizing to group functioning, so they must be labeled harmful in order for said society to survive and thrive, and psychiatry is a part of a system that perpetuates and reinforces that labeling. In turn, as a future psychiatrist, I feel my loyalties divided: I know how important it is to have evidence-based reasoning and framework when I approach problems and patients, but much of that evidence comes from a very confused, and often cruel, history, representative of a time that doesn’t even remotely reflect my current beliefs. In my training, I’ve found that this kind of dilemma is rarely, if ever, addressed.
I know there aren’t any easy answers to be had here, but I’m curious if others have had similar thoughts, and how they’ve navigated those dilemmas. On the more practical side, did you ever feel conflicted about reconciling your responsibility to the legacy of your specialty versus making a diagnosis that could impact the future of your patients? I have a feeling, as with all medicine, that it’s a case-by-case basis, but I hope that it’s something that we all continue to consider from time to time. I think that it’s easy to forget that we are the gatekeepers of normal, and that during every diagnosis, treatment, and discussion that we have, in private or in public, with patients, friends, and family, we are constantly exercising that power of opening and closing that gate.
How do you balance being a "gatekeeper of normal" in your medical practice? Share in the comments.
Tim Hsu, MD is a big ball of yarn. He spends most of his time being batted around by his cat. In his free time he reads, plays video games, and occasionally gets some work done. You know, just a typical psychiatry resident. He is a 2020–2021 Doximity Op-Med Fellow. Dr. Hsu has no conflicts of interest to disclose.