During my surgery rotation, I learned that every operation is different, but the lead-up is often the same: Read the board. Stand still, out of the way, as the screen flashes through all twenty-five operating rooms, five at a time. Find out when your case is, where your case is, and maybe (as an afterthought) what it is. Don the scrub cap and the shoe covers. Put on a mask. Make sure you grab the one with an attached face shield, because even if this case does not require eye protection, that determination feels far too complex to make with any confidence. Enter the operating room briefly to grab two pairs of gloves in your size. Introduce yourself to the nurses. Take care to emphasize not your name, but your role. “Medical student.” They will lower expectations accordingly.
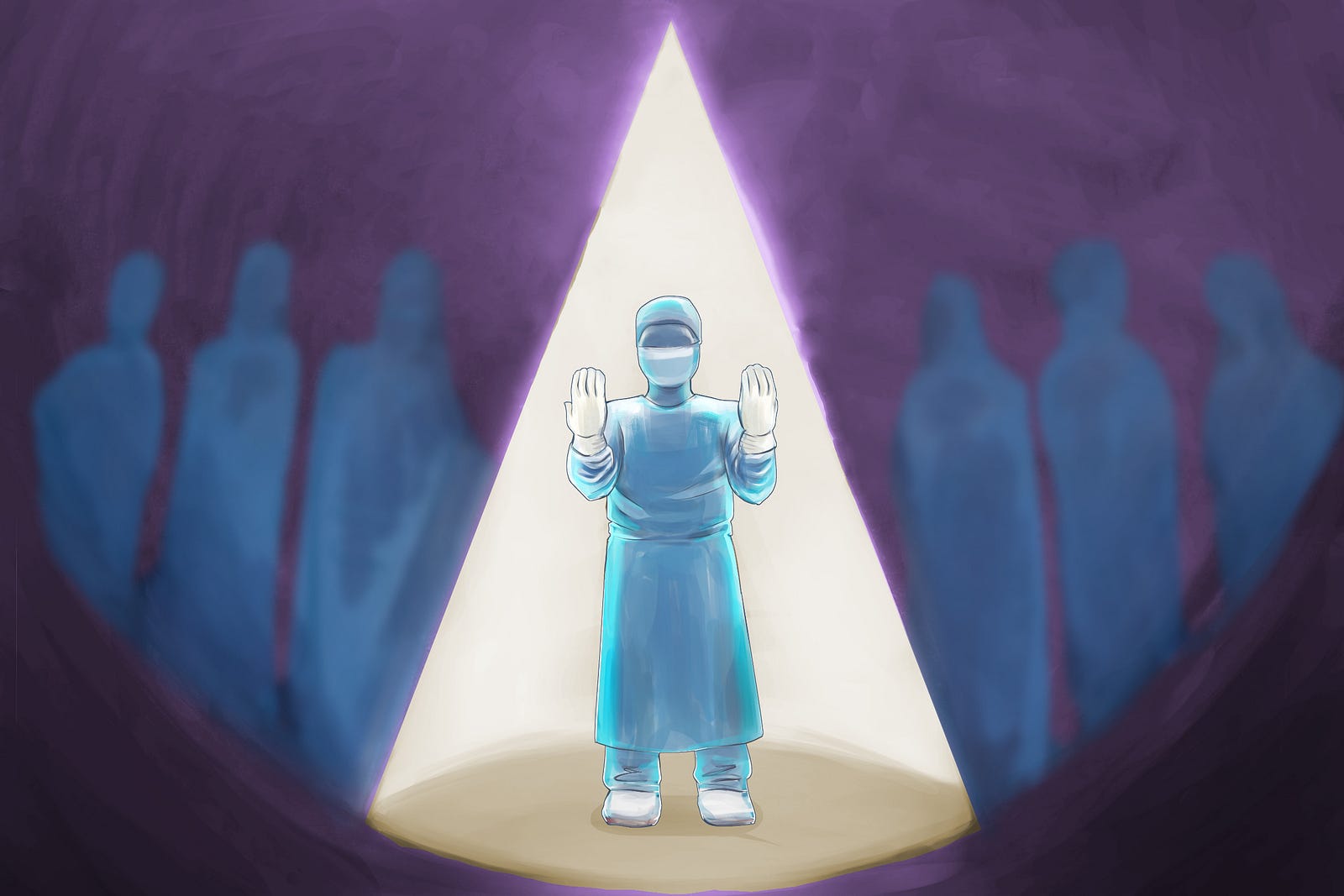
When it is time to scrub in, be fastidious. Leave no speck of fingernail dirt behind. Grace every surface of your fingers, hands, and forearms with the detergent-impregnated sponge. Count to 180, or when you inevitably lose track, settle for counting to 50 at least a few times. When you re-enter the OR, kick the door open with your foot. Stand with arms flexed in front of you and wait for someone to hand you a gown. Expect to wait just long enough that you start to question whether you are invisible. You are not invisible; you are just unimportant. With time, that may feel comforting.
Don the gown. Let your fingers emerge from the sleeves and then put on your first pair of gloves. Put on your second pair of gloves. Say a prayer to whatever deity you might imagine resides in that sterile room: that you do not find your nose itching, that your mask does not start to creep toward your eyes and obscure your vision, that your neck will not be so awkwardly strained in downward flexion that you wake up sore the next day. Thank the deity for the fact that a mask, at the very least, makes it easier to conceal your yawning in the fifth hour of the case.
There is a reason the phrase “operating theater” has persisted. This is a production. You play a bit part.
You might expect that as a medical student on a surgery rotation, you would be most concerned with preoperative testing, anatomical landmarks, and laparoscopic techniques. Certainly, these things matter. Yet in the first few days, what seems to matter far more — and demand far more of your mental energy — is memorizing the choreography of that initial dance.
On day one of my surgical subspecialty rotation, after making it through the routine with more blunders than I care to admit, I found my gloved hands making their way toward my masked face. My gloves were sterile; my mask, though clean, was not sterile. A mixing of the two would be unacceptable. A nurse in the room looked at me with a crinkled brow, but kindly eyes.
“Did you just touch your mask?”
I was silent and contorted my own face, too, as if the question were far more complicated than a simple yes or no.
“Because if you did, you’ll have to scrub in again.”
I adamantly shook my head in denial.
“Are you sure?”
I nodded. She looked unconvinced, but nodded back at me and continued about her tasks. I took my place at the table, hands poised above the patient, ready to hold whatever suction or retractor came my way. I tried to replay the events in my mind, frame by frame, pausing when I reached the moment where my fingers jolted back to my sides after coming perilously close to my mask. I had not, in fact, broken with protocol; I had not contaminated the procedure. I was still on script.
Yet the greater revelation was that, had I erred, I was not certain I would have been willing to admit it. I like to believe that I am a humble person. And yet, I would have been too proud to acknowledge failure before the operation even began.
For days thereafter, I read the notes in the patient’s chart obsessively, attaching meaning to even the most nominal spike in temperature or rise in heart rate. Tenths of a decimal and couple of beats per minute notwithstanding, his progress notes told a soothing story. Day 1: stable vital signs. Day 2: “NAEON,” the nurse had charted. No acute events overnight. Day 3: patient cleared for discharge. I had done nothing wrong, and the patient’s uneventful post-operative course proved my point.
I want to be a doctor because I want to help people; this rationale is equal parts hackneyed and true. The path to this aim, however, is murkier than I anticipated. It involves messing up in small and large ways over and over again, and it involves choosing each time to stay silent or to acknowledge and learn from a mistake. I have been told that a good surgeon is often wrong but never uncertain, and this mentality makes sense in the quick-paced environment of the operating room. Yet if we take this too far and refuse to own up to mistakes, we reinforce the flawed notion that vulnerability is weakness. We stand the chance of allowing hubris to take precedence over patient care.
If we truly want to help people, this is not a risk we should be willing to take. Instead, we should acknowledge that sometimes, even the oldest scripts need to be rewritten.
Gabriela Reed is a medical student at the University of North Carolina, anticipating graduation in 2019, and currently deciding between family medicine and internal medicine.






