Background
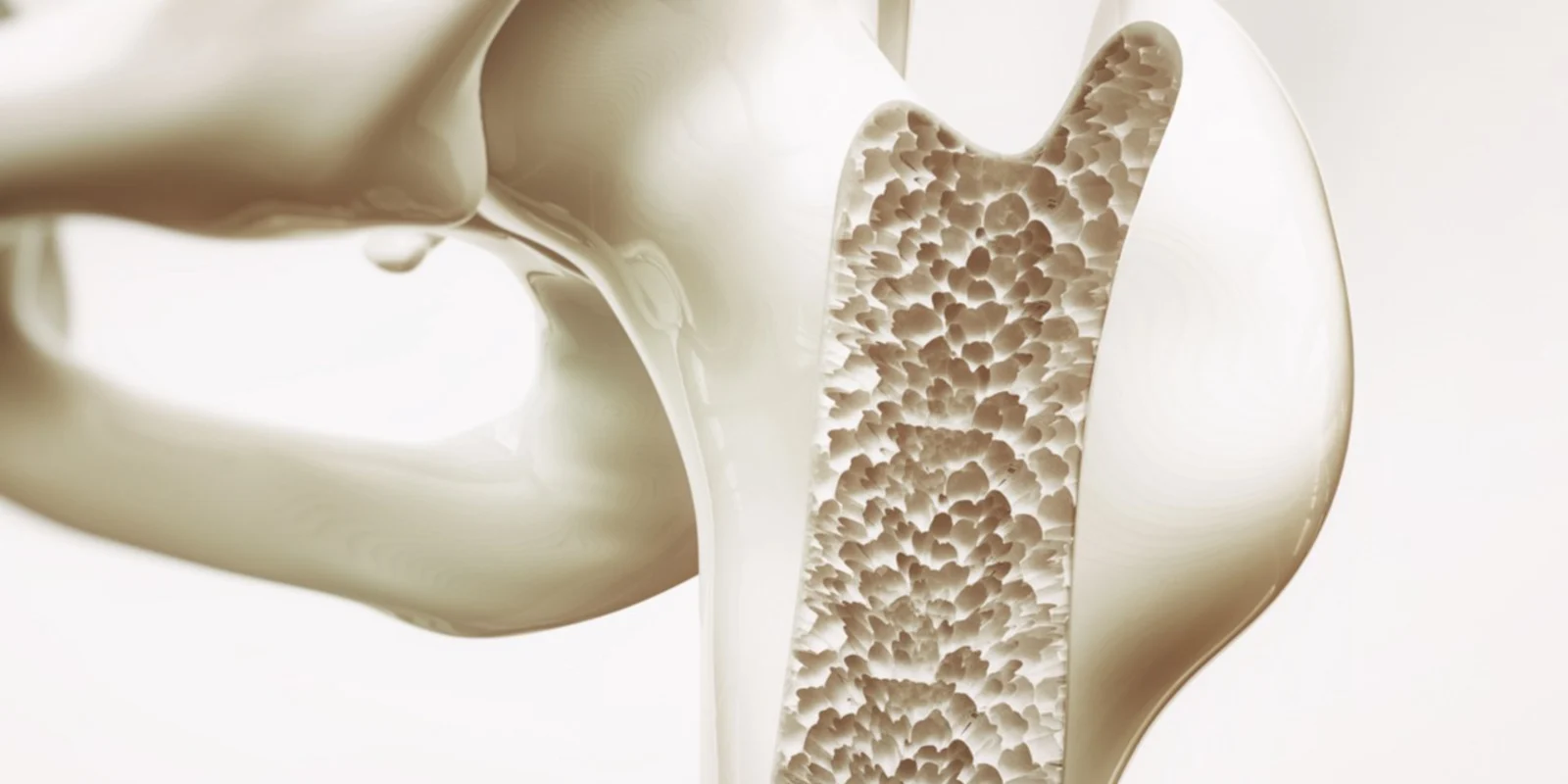
Osteoporosis and osteopenia have been estimated to affect over 50 million Americans. These silent diseases of low bone density often go undetected until a fragility fracture occurs — an injury that can sometimes prove to be debilitating for vulnerable patient populations. For this reason, the USPSTF recommends bone density screening for women aged 65 years and older and in younger women with additional risk factors. Most commonly, initial bone density measurements are done via dual energy X-ray absorptiometry (DEXA) scans. DEXA scans are ordered in the offices of primary care doctors across the country as part of routine screening.
Likely for this reason, updated clinical practice guidelines for the treatment of low bone density were published by the American College of Physicians (ACP) in the Annals of Internal Medicine this past summer. Summarized in this table, the guidelines are intended to direct general internal medicine practitioners in their diagnosis and management of osteoporosis.
But while these guidelines brought with them increased awareness of the importance of screening for and treating low bone density, they also came under heavy scrutiny by experts in the fields of rheumatology and endocrinology.
The Issue
In an editorial piece for the official journal for the American College of Rheumatology, Arthritis and Rheumatology, experts applauded the ACP’s focus on an often overlooked disease process, but they also questioned several of the guidelines made by the group. The ACP’s first-line recommended therapies left off several medications, such as ibandronate, raloxifene, and teriparatide, all of which have been approved for osteoporosis management.
Experts also called into question the recommendation to treat for 5 years; certain clinical scenarios may call for fewer or more years of treatment. The ACP’s recommendation to not repeat DEXA scans for the duration of this five-year treatment period came under fire as well. Many endocrinologists I have spoken with check DEXA scans annually in their patients on pharmacologic therapy, consistent with the American Association of Clinical Endocrinologists (AACE) recommendation to monitor treatment response with DEXA scans every 1–2 years.
While the jury may still be out on appropriate screening intervals and treatment duration, it goes without saying that osteoporosis diagnosis and treatment can be highly nuanced. More rigorous discussion and consensus guidelines are needed to help best frame osteoporosis diagnosis and management for the internist. And complicated cases of low bone density may often require subspecialty care, so referrals should be made accordingly.
Looking Forward
But, perhaps before even getting to the question of DEXA scans and low bone density, patients may ask their provider: “Well, what about vitamin D and calcium supplementation?” Up until recently, evidence had mostly been inconclusive regarding the benefits of calcium and vitamin D for prevention of osteoporosis-related fractures.
A recent systematic review and meta-analysis in JAMA aimed to bring a little more clarity to this issue. Their analysis included 33 randomized clinical trials that incorporated over 50,000 participants. Compared to placebo, they did not find any significant difference in the risk of hip fractures in those taking calcium and/or vitamin D supplements.
When abaloparatide was approved by the Food and Drug Administration (FDA) in 2017, after the success of the Abaloparatide Comparator Trial In Vertebral Endpoints (ACTIVE) trial, it was the first new osteoporosis drug to be approved in nearly 10 years. Osteoporosis treatments seemed to herald a new favorite with romosozumab, a monoclonal antibody that binds to and inhibits sclerostin thereby stimulating bone formation and inhibiting bone resorption. The Active-Controlled Fracture Study in Postmenopausal Women with Osteoporosis at High Risk (ARCH) study was published in the New England Journal of Medicine in the fall of 2017. While the study clearly demonstrated the superiority of romosozumab followed by alendronate compared to alendronate alone in fracture risk reduction, it also noted an unexpected increase in cardiovascular events in the romosozumab group.
Due to these concerns regarding cardiovascular risk, this past summer the FDA rejected romosuzumab, with a request for additional study data to further investigate these safety issues. In the meantime, providers can continue to screen for low bone density with DEXA scans per the current USPSTF recommendations. New treatment options may emerge, but the current arsenal of treatment options includes oral and intravenous bisphosphonates, parathyroid hormone analogues, and monoclonal antibody therapy. Future clinical practice guidelines may also help streamline diagnosis and management, hopefully with more consensus amongst general medicine and subspecialty physicians.
Farah Naz Khan is a doctor and a writer. She is a 2018 Doximity Scholar. Find her on Twitter @farah287 or via her website, FarahNazKhan.com.