COVID-19 is a global pandemic, and as of March 25th, 2020, there are over 400,000 confirmed cases. Just in our state of Florida, there are nearly 2,000 total cases. I would like to implore residents and fellows to approach the pandemic with these three immensely essential questions:
- How can we protect ourselves while still providing exceptional patient care to those in need?
- How can our fellow/residency program protect us?
- How can our hospital protect us?
There has been nothing like this pandemic in our short time as physicians, and now is not the time to be quiet in advocating for your patients, as well as your well-being and safety.
How can we protect ourselves while still providing exceptional patient care to those in need?
The number one recommendation to tell anyone who wants to protect themselves from this virus is to wash your hands and avoid exposure to others. The second part is impossible as clinicians, and thus other steps are of utmost importance. Wear a mask if a patient has a concerning presentation (cough, shortness of breath, fever, myalgias). Do not hide your symptoms if you are experiencing any similar symptoms yourself. This is not the time to be a hero. Do not expose yourself to a patient’s room unless completely necessary for adequate care. Attempt to limit the number of residents that see the same patient. This may mean staffing the intern’s patients with the attending physician for the time being. Encourage everyone to chart review from home, as any way to spend less time in the hospital is a good idea. Lastly, do not agree to provide care outside of your education. Please, fellows and residents, realize the severity of this disease. Take care of yourself.
How can our fellow/residency program protect us?
The number one recommendation for our program to protect us is to limit resident-resident exposures. All in-person didactic lectures should be canceled until further notice. These can be continued through online meetings or implementing required quizzes through a service like MKSAP. Residents should also not be required to come to the hospital for any reason other than if on an inpatient rotation.
Ensure our well-being and be our advocates. Everyone reacts differently to life-threatening situations. This is a very stressful time and a new experience for all of us. If a resident admits to worsening mental health due to COVID-19 hysteria and seeks aid — no penalty to this resident should be enforced if time off is requested. This includes, but is not limited to, an extension to residency training or monetary restriction. Also, please remember we do not know all the rules and restrictions of the hospital or corporation we work for. However, we do expect our residency program to keep us up to date as this pandemic evolves.
These measures are fundamental to ensure our safety, as this should be the number one priority of the program. Here is my contingency plan that should be in place and can be extrapolated for all residencies.
My recommended approach for a contingency plan is to cut elective rotations until COVID-19 control has been established. Here is an example for an internal medicine residency, as follows:
Let’s say that your residency program has 60 internal medicine residents. Current rotations include the following:
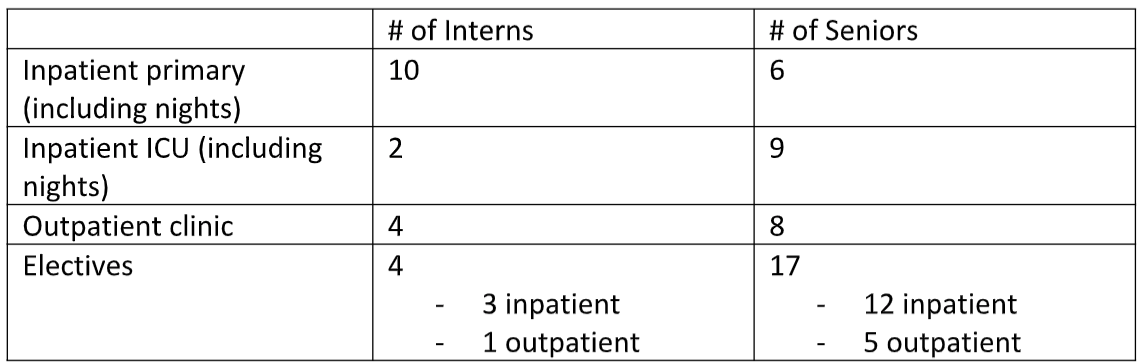
This table shows that 21/60 or 35% of residents are on electives. These 21 individuals should be sent home for the next two weeks. They should not be required to take PTO, sick leave, or have an extension to their residency training. Let me explain. In this example, 70% of the residents are involved in inpatient rotations. What is to happen if these individuals are exposed to the virus? There is at least a five-day incubation period before symptoms develop. That means it will be about a week until an individual realizes that there is something wrong. During this week, each resident will not only expose his or her patients but will also expose his or her co-residents to this virus. In other words, once the symptoms develop, 70% of the residency program will require quarantine, and, therefore, cannot safely see patients.
Therefore, sending home residents on electives will cut in half the number of residents in the hospital at one time. Sustain at least 21 residents to be available for inpatient care if the current team is exposed to COVID-19 and requires quarantine. We will call the quarantined Team #1 and the inpatient Team #2. If all goes as planned, Team #1 (those on electives that had the first two weeks off) would switch with the current Team #2 at the 14-day mark. This will ensure that the critical rotations of an internal medicine residency (inpatient internal medicine and intensive care) are covered as this virus grows exponentially.
Lastly, please do not:
- Push us to work outside of our scope of practice.
- Allow our workplace to threaten our safety.
- Force us to be on call 24/7.
- Take our vacation time away if we are required to work despite approved PTO.
- Make all residents work at one time.
- Forget that social distancing is also crucial for us.
- Force us to work if we have symptoms of fever, shortness of breath, or cough.
- Forget that this is out of our control, and that we should not be penalized for that.
As a resource to the graduate medical education community, the ACGME has shared a statement from the American Board of Medical Specialties to designated institutional officials regarding coronavirus (COVID-19) with a similar sentiment: "..boards are supportive of creative strategies to recognize learning opportunities that can take place during such times. In situations in which quarantine impedes completion of on-time training, boards are receptive to case-by-case discussions and do not wish to penalize trainees for situations beyond their control."
Please, fellow/residency programs, realize the severity of this disease. Do not subject us to useless exposures to fulfill a quota. Accept a stain on the perfect residency record. Please do not risk our lives.
How can our hospital protect us?
We need personal protective equipment in stock and readily available to us. This includes, but is not limited to, skin protectants, eye shields, gowns, masks, and air-purifying respirators. Without this, we are sitting ducks to contract this life-threatening virus. We need to cancel all elective procedures, limit visitors, and entry points into the hospital. Appropriate screening by qualified medical personnel must be completed. If any hospital staff were to become sick, there must be an alternative ready to fill that spot immediately. One specific example would be respiratory therapists, as they are vital to the proper management of the ventilators.
Telemedicine must be used as much as possible. At the current time, there is genuinely no reason for a patient to come to the clinic for a refill of their medications they have been on for years unless there is a specific change that needs to be addressed. These encounters should be virtual through telemedicine. If a narcotic script is required, the patient can come in and pick this up without spending needless time in a high-risk area. Keep our seniors at home.
In the case of a positive COVID-19 case, there must be an attempt to obtain a HIPAA form signed by the patient to allow at least the hospital staff to be aware. We cannot allow our staff to walk into an area with this virus, and unknowingly become infected and cause further dissemination. The positive case should be isolated in a private room with all necessary measures to prevent further spread.
Please, hospital board members, realize the severity of this disease. Our bodies require oxygen to survive. Patients require a hospital’s critical resources to survive. Our bodies will not survive without oxygen. Our patients will not survive without hospital resources. We are fighting against a pandemic, now is not the time to be frugal.
To finish, let me explain why hospitals and residency programs should consider providing extra stipends to their trainees.
Italy is showing that one of the most vicious risk factors of death from COVID-19 is overworked front-line physicians. We, as residents, are typically working 80-hour work weeks. We will continue these during this pandemic, exposing ourselves every day to a potentially fatal virus. Is this any different than other exposures on an everyday basis in the hospital? I would say yes. Not every day are the top medical conferences, sports associations, universities, high schools, medical schools, day cares, and stores closing and canceling. It is easy to see that we are willingly exposing ourselves to this pathogen, as patient care is our number one priority.
The economy is in turmoil. We are paying more for unfamiliar daycares for our children while we work. Some of us are living in Airbnbs because we cannot come home to our compromised spouses and children after potential exposure. We will be working long days and may potentially be quarantined in the hospital. The stipend should be considered for us, similar to an employee’s hazard pay. I understand that this may get a laugh from hospital CEOs. Nevertheless, I would remember, if a resident physician becomes sick at your hospital and dies, how is his or her family going to live? We pour our entire hearts and souls into being doctors. Any extra monetary assistance in this unfortunate time would be beyond beneficial. Who knows? Maybe it will lead to the retainment of a physician or two after graduation.
We are in the exponential growth phase of this pandemic in the United States.
It is our job as young physicians to not only treat this disease but to do our part to contain it.
Dr. Alexander D. Lake, DO, is a PGY-2 internal medicine physician in Hudson, FL. He is the Chair of the Florida Medical Association Resident and Fellow Governing Council.
Click here to see more perspectives on COVID-19 from the Doximity network.
Click here for up-to-date news about COVID-19 on Doximity.