Emergency medicine is a difficult field. It can be exciting yet stressful at the same time. You never know what will present next. It can be the most minor of complaints such as a paper cut or it can be a patient at death’s door. One would think that the latter would be the hardest patient to treat, and although those situations can be difficult, the diagnosis at least can be a lot easier. It’s a lot harder to figure out the patients who don’t look that sick but can end up dying at any minute. That’s the first major mistake that I know that I’ve made.
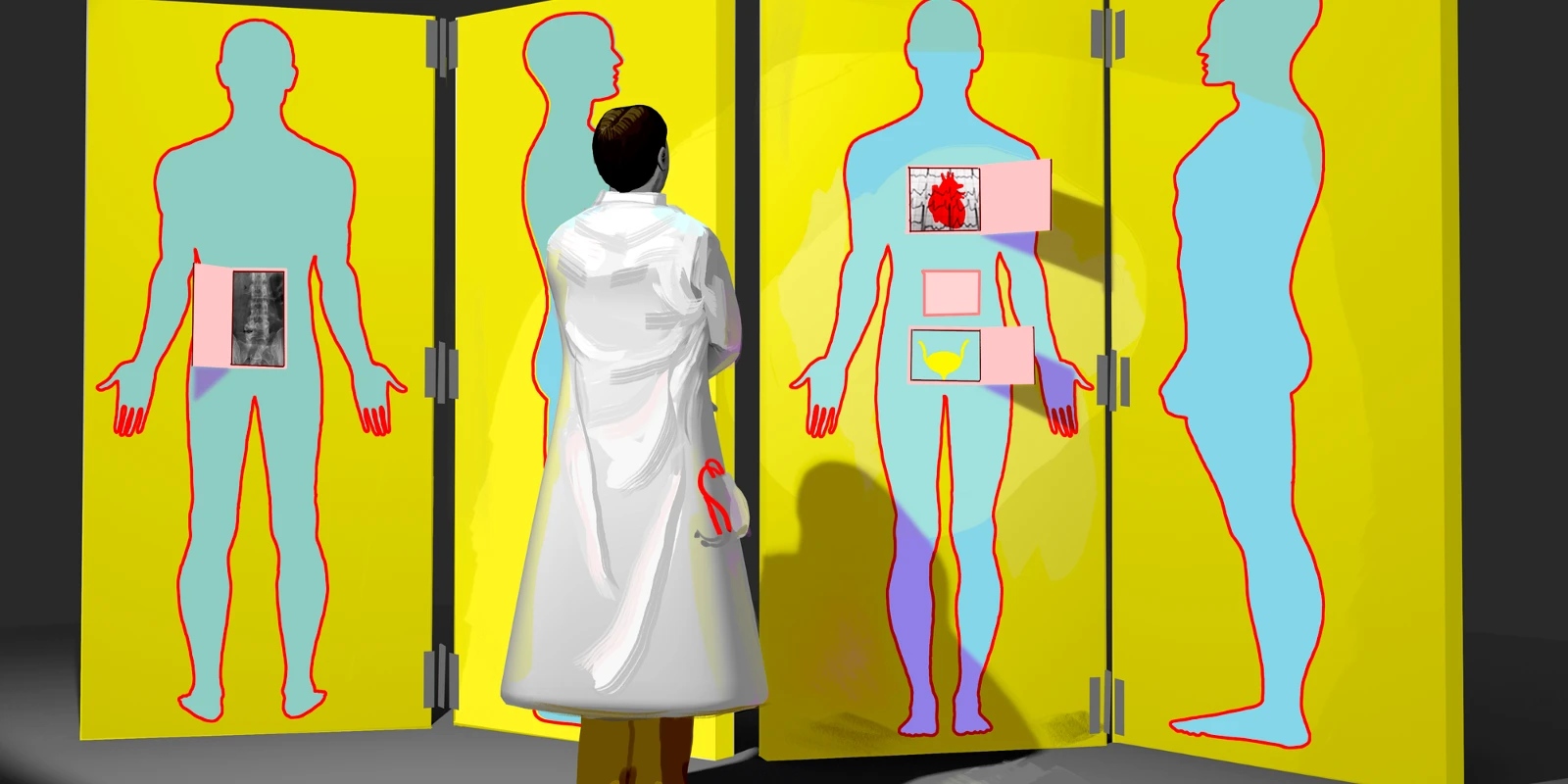
He was an elderly white man who lived alone. The complaint was back pain, and like many older people, he had other health issues as well. He was on warfarin for atrial fibrillation and also had a history of high blood pressure. He said he had woken up with the back pain during the night and had trouble sleeping because of it. He walked into the emergency department, and his vital signs were all normal. He mentioned he might have some abdominal pain as well, but the back pain was his main focus. For a weekend morning, it was decently busy and though, like one of my mentors had taught me, I thought of some of the life-threatening diagnoses that I needed to rule out, this guy looked pretty good overall. I did some basic bloodwork and ordered some X-rays of his back. I did a brief exam of his abdomen with the ultrasound machine, but as he wasn’t thin, didn’t get a clear view of things but didn’t see a lot that generated interest.
I went off to see some other patients, and when I went to check back on him, he seemed to be doing OK. I had given him some acetaminophen for his pain, and he seemed better. His lab work wasn’t entirely normal but nothing that seemed too exciting. His INR was a little high and he had some blood in his urine but I attributed the latter to the former. His vital signs throughout the ED stay remained normal. His lumbar spine X-rays had been read as normal by the radiologist. I mentioned to the patient that he had some mild lab abnormalities and instructed him to follow up with his regular doctor, and I even watched him walk before putting the discharge order in the computer.
I continued on with my shift, but then received a call from another hospital nearby where I was doing my fellowship. After I had discharged the patient home, he had collapsed outside his apartment and an ambulance had been called and brought him to the other hospital. They were trying to figure out what was going on but had seen he had just been the hospital I had been at and were trying to piece together what happened. It turned out he had ruptured his aorta and though they were able to keep him alive to the ICU, he died shortly later. Even if I had made the diagnosis that AM, he might have died, but missing the diagnosis, and the resulting consequences, obviously made me very upset.
The ironic thing is I even had thought about the diagnosis of an abnormal aorta. Unfortunately, I didn’t get a clear view on my ultrasound exam, and though I considered doing a CT scan on him, he didn’t seem that sick. I have to admit, it crossed my mind that the hospital was keeping track of how often we were ordering more expensive imaging scans, and wanted to make sure we weren’t ordering too many. Later I looked at the actual X-ray of the gentleman’s back and it was clear that his calcified aorta was ballooning out on the X-ray. And in retrospect, the last set of vital signs that the nurse took after I had put in the discharge order was abnormal, but I was never informed about them.
The case was brought up appropriately for M&M rounds, which I attended, and it was stressful to have the case reviewed. I had recently finished my emergency medicine residency, which had been extremely tough, but I was reasonably confident it had left me a competent physician. I definitely learned several things about the case — not to hesitate to order imaging studies on older patients, to be more aware that older patients can hide pathology, and to make a better effort at looking at the radiology images myself, to name a few.
These days, most M&Ms are kinder and in some places, they don’t really have them anymore. They are replaced by Quality Assurance rounds and similar names. And there is a lot more awareness of biases that leads to errors and systems issues that allow mistakes to occur. That being said, I still feel there is a need to take personal responsibility for errors, if only to remind that indeed, I am human.
The author is a practicing emergency physician.