“Can we just scan my abdomen, just to check that everything is OK?” My patient was worried about her risk of pancreatic cancer after her neighbor had passed away from the disease. Despite her lack of symptoms, she felt an MRI would offer “peace of mind.”
I explained that, unfortunately, we didn’t have a good way to screen for pancreatic cancer.
“I would feel a lot better if I could get an MRI,” she said. “And don’t you think that it’s better to check now than to catch the disease too late?”
Full-body MRI was something I had only heard about in the context of Li-Fraumeni syndrome — a rare disease that dramatically increases your risk of cancer. A radiologist in medical school described the surveillance protocol at that time: full-body MRI scans every six months, with radiologists carefully monitoring and measuring every slight abnormality over time to see if it was cancer. It was an extremely labor-intensive process.
Recently, direct-to-consumer MRI services have sparked public interest. For a fee ranging from $650 to $2,500 (depending on the company and tier of scan), a person can receive a one-time, full-body MRI scan. A radiologist interprets the scans, and the results are sent to the patient, sometimes in conjunction with a consultation by a staff doctor. Most companies offer to send a report of results to the patient’s primary care doctor.
Despite the hype, there are real risks to these practices. First, scans lead to incidental, indeterminate findings. Known as “incidentalomas,” these are radiographic findings that could be something worrisome like cancer but equally likely could be a myriad of other benign findings like inflammation, infection, vascular structures, etc. One study suggests that the prevalence of incidental findings across CT scans is as high as 31.3%. Incidentalomas present a management dilemma due to the lack of clear guidelines. Sometimes, doctors manage with regular surveillance. Other times, the decision is made to pursue biopsy to better characterize the finding.
In both pathways, there are tradeoffs. In surveillance, doctors must decide when and how often to reimage — often with limited guidelines. Further imaging often requires radiation exposure. How many cancers will be caused by subsequent radiation after a full-body MRI?
Moreover, the EHR is not equipped well enough to organize this information over time, increasing the risk of oversight. Primary care doctors, already stretched thin, bear the brunt of managing follow-ups for these findings.
Additionally, following up incidental findings can bring real harm. Biopsies are invasive tests with surgical risks of complications.
One patient of mine was incidentally found to have slight leukocytosis (high WBCs). This led her down a long road of lab tests, multiple invasive biopsies, and expensive consultations with specialists. When finally she came to my clinic, it was after a five-plus year hiatus at doctors’ offices because she had too much anxiety and PTSD to go to a medical facility. When I brought up the WBC lab result with her, she burst into tears and urged me to just leave it alone.
Some risks are more difficult to quantify. One patient’s well-meaning parents pushed for a heart ultrasound (transthoracic echocardiography) because of a distant family history of heart disease. The ultrasound revealed a very slight thickening of part of her heart wall. Her cardiologist emphasized that these results were clinically insignificant. Despite this, she was denied for disability and life insurance multiple times because that record was in her chart.
Still, I can’t deny that well-timed scans could save lives. One patient of mine was in her 40s when she presented to the ED for abdominal pain and was found to have diverticulitis. But the abdominal scan caught part of the lung, which led to a diagnosis of stage 1 lung cancer — and subsequent resection and cure. In my office, together, we marveled at the series of events that led to catching her cancer. She didn’t meet the guidelines for screening as someone who had never smoked. There is a reasonably high chance that she would have died from lung cancer had this scan not been done.
Moreover, there is a stark dichotomy in access: Affluent individuals can afford elective scans while my low-income patients struggle to obtain necessary medical care. MRIs in particular garner significant gatekeeping by insurance companies. I have spent hours dealing with insurance companies trying to get an important MRI covered for a patient.
Public sentiment, however, seems to be markedly positive. A recent news article on an MRI company garnered dozens and dozens of comments heaping effusive praise on the scans. The consumer-driven demand for health data is not new. Many states allow patients to get a lab test without a doctor’s order. Companies capitalizing on this offer a range of blood work, including common tests (e.g., complete blood count, basic metabolic panel, and urinalysis) with costs ranging from $50-$200. Some offer panels to assess “fertility,” or “men’s health.” Access to tests mirrors the 21st Century Cures Act, legislation that mandates medical practices gives patients access to their medical records. It seems that patients want more data and more access to their data.
Often quipped in the tech industry, the saying, “The future is already here, it just isn’t evenly distributed” applies to medicine, too. Is more and regular imaging the future? Many (albeit not all) of the problems with full-body MRIs are issues of resource allocation and cost, and can be mitigated with close follow-up and careful counseling. For those for whom this is not an issue — like the celebrity Kim Kardashian — regular MRIs and subsequent clinical management is already part of their wellness routine.
Proponents argue that, although right now these companies are only in the purview of those with resources, increased use of the technology will lead to better outcomes data to reduce false positives. And as MRIs become more widespread, it could lead to cheaper and better technology, ultimately reducing the cost of these machines.
The growing enthusiasm for full-body MRIs reflects a trend in health care: the proactive pursuit of wellness through personalized data. While the allure is understandable, it must be balanced with the reality of medical risk and resource allocation. We strive for a health care system that is equitable and evidence-based while also acknowledging and seeking to incorporate evolving technology and patient preferences.
How do you address unnecessary medical testing? Discuss your approach below.
Corinne Carland is an internal medical resident at the University of Pennsylvania in Philadelphia. She is interested in health tech, clinical informatics, cardiology, and genomics/proteomics. Outside of work she enjoys walking/running along the river, trying new ice cream spots, and exploring museums. Dr. Carland is a 2023–2024 Doximity Op-Med Fellow.
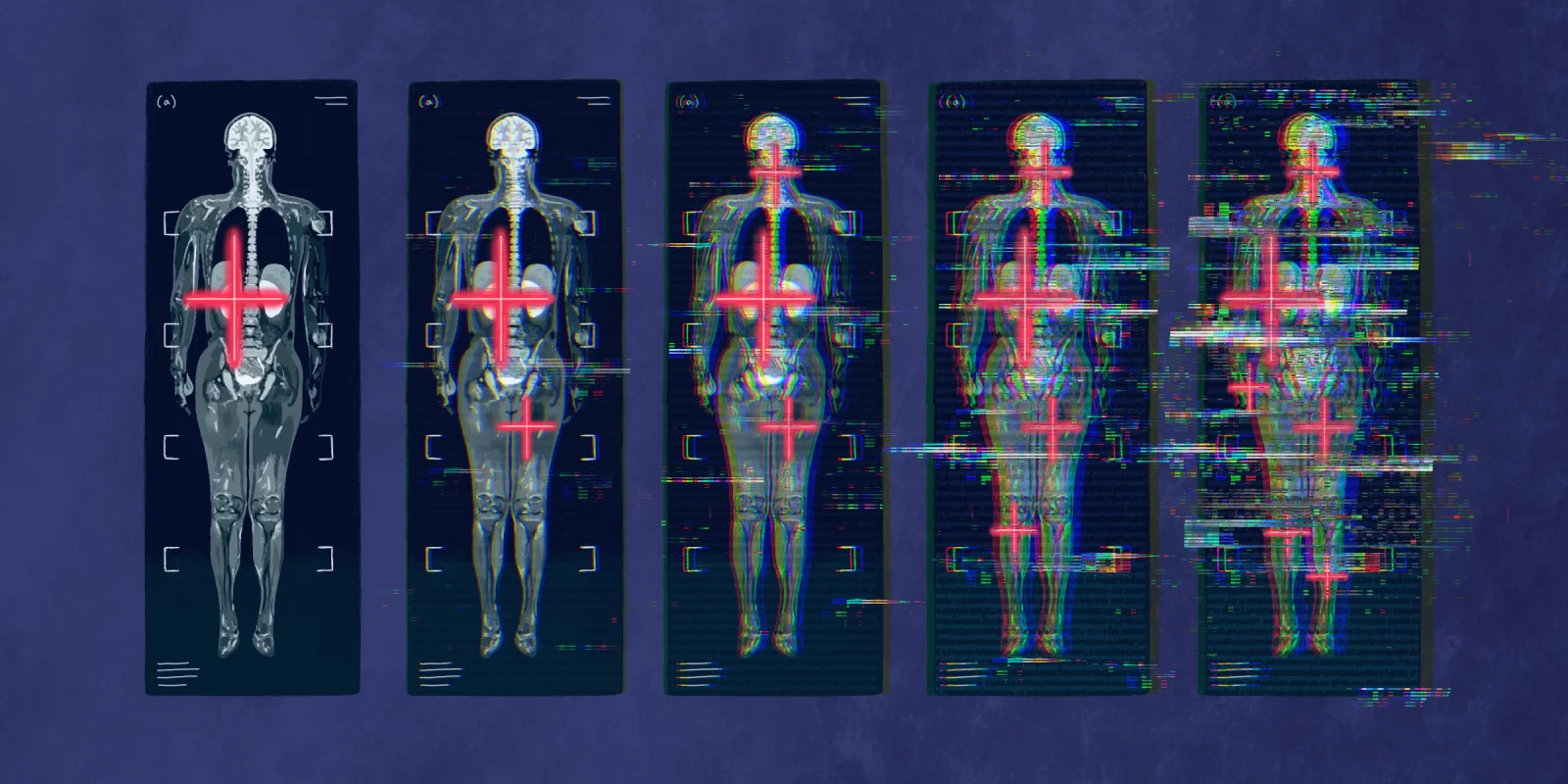
Illustration by Diana Connolly