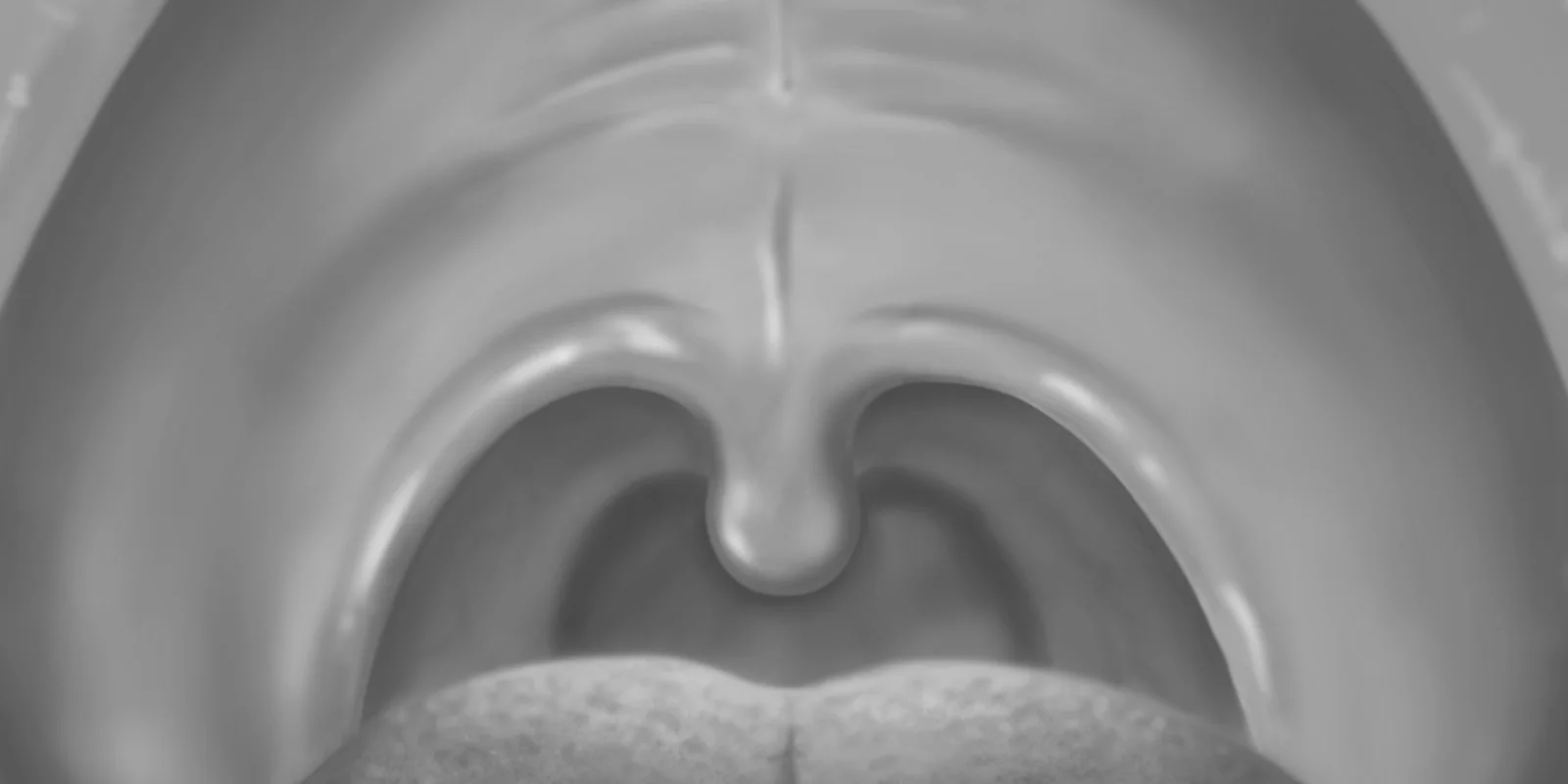
I recall the exact day that the light of my otoscope reflected on what appeared to be a small bunch of grape-like flesh-colored tissue on my patient’s uvula. The small cluster took me by surprise as I was examining my patient for the chief complaint of possible strep throat. On the left side of the uvula, the fleshy mass mimicked common pinkish lesions I often see when doing Pap smears. Could it be? Is it? HPV? At that moment in time, I realized that my patient was going to be diagnosed with more than pharyngitis but that my possible new diagnosis will have lifelong implications for cancer risk for him. My mind raced as I searched for the right words to tell my patient at the end of this encounter. Life changing words.
I shivered again as I prepared to discuss a possible case of what looked like HPV on the uvula and the risk factors for throat cancer if it truly is this pathogenic DNA virus. This looming diagnosis if confirmed by the ENT doctor will create a dark cloud of possible throat cancer risk for the rest of my patient’s life. Only recently the medical community has been shaken with celebrities developing HPV related throat cancers in their fifth decade. Fortunately, the future of our teenagers will be less stricken with throat cancer risk due to the release of the HPV vaccine in 2001.
I wondered if my patient’s risk for throat cancer will be compounded by his history of smoking, oral sex, and alcohol use. With many more patients choosing not to purchase insurance the preventative exams are not first choice measures to be paid to have on a regular basis. Many times our male patients only come to the clinic when they are very ill. How often do practitioners do a thorough oral exam? Do practitioners examine the mouth in the patient coming in for STD treatment or birth control? Are we guilty in the medical community at missing screening opportunities for our sexually active patients for HPV-related lesions in the oral mucosa? What about our female patients who come to us for their annual breast exams and Pap tests; are we checking their oral mucosa as part of the exam?
The medical community maintains that 85% of the time HPV can clear within months but only recently do we understand that the virus can lie dormant in the skin cells for a lifetime. Therefore, is the risk minimalized or are we waiting for the ‘great disaster’ to hit in our fourth and fifth decades with soaring cervical cancer rates or now, throat cancers? DNA testing is costly and we co-test on Pap tests in our female patients over the age of 30 years but what about routine screening for the oral cavity? Is it possible to use the co-test on the throat as an accepted guideline?
I am not sure if science has imprisoned this felon virus, HPV, in adequate time to prevent possible soaring rates of throat cancer in the ‘Latch Key’ or ‘Millennial’ generations. Baby boomers are currently being treated and diagnosed now with HPV related throat cancers but HPV exposure would have been more minimum in that generation. In fact, the discovery of HPV was only in 1956 and not until 1984 did Harold zur Hausen clone the HPV virus and attribute cervical cancer to be caused by the HPV viruses 16 and 18. Following the trend in the evolution of common DNA virus mutations lies the fear that these organisms are capable of changing and wreaking destruction in future generations. A mad scientist would argue that the HPV DNA viruses are ‘part and parcel’ of the expectations for mutant viruses to demolish and wreak havoc on human immune systems in the future. Theoretically speaking, the “time capsule” for the prediction of future worldwide HPV cancers will depend on the effectiveness of current HPV vaccines, accessibility, and the ability of the DNA viruses to mutate. This paradigm reminds me of the WHO so-called eradication of the smallpox virus in 1980 yet with the looming dark cloud of Russian and Siberian scientists concerned about a possible return of the virus. As a practitioner, I hope that the future Generation Z will never have to experience family and friends dying of HPV related diseases and as the smallpox virus, will be eradicated in my lifetime.
Would my patient’s life be any different if I had seen him 3 months ago? Would the ‘Case of the Surprising Uvula’ have even existed at that time?
Connie Lapadat, NP, is a family nurse practitioner in El Cajon, CA. She is also a 2018–19 Doximity Author.