The Dox Foundation ran a Global Health writing contest in September 2019. We are excited to announce this as the winning piece.
“She doesn’t need to know,” Thambi said, his black-brown eyes holding mine defiantly. He was my age, with dark skin that contrasted with a dirty white shirt that was too big for him.
I leaned forward, hoping my frustration could not be seen in my posture or face. There were 8 of us sitting shoulder to shoulder in that tiny examination room in India. It was stifling hot, the smell of body odors mixing with the sterility of a hospital. The window was not big but I looked past the bars to the garden beyond and willed for a cool breeze to blow through.
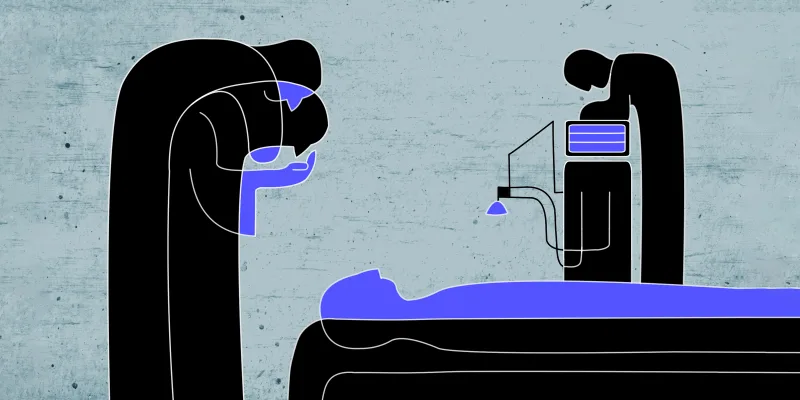
Thambi’s mother, Mrs. Kani, curled to her side on the examining table in the corner, her head turned away. She was skin and bones with a faded yellow sari draped over her. I reviewed her chart again.
Seventy-three years old. Widowed. Metastatic breast cancer. Mastectomy, chemotherapy, radiation. Relapse. Treatment failure. Fungating mass.
I put the file down and went to Mrs. Kani and I laid my sweaty palm in her hand, which was cold and rough. She curled her hand over mine and squeezed ever so lightly. I saw a woman that had questions, fears, and hopes, and yet she clenched her teeth and shook her head softly.
“I don’t want to know. I want you to speak to my son — he will tell me, if he chooses,” she said.
I stood up quickly and nodded. I escorted the family into another room so we could finish the conversation about Mrs. Kani’s health; about the progression of her cancer and the unlikeliness of cure. Thambi nodded, and asked about anything else that could be done to cure her. I spent the next hour answering questions from the family and telling them about palliative care.
“I see that you love your mother very much and are trying to protect her,” I said. Thambi swiped the back of his hand across his unshaven cheek, stood up, and left the room.
That was four years ago when I went to India as a volunteer to a palliative care hospital in Salem, Tamil Nadu. I came home and wrestled with that encounter. Mrs. Kani obviously knew that she was very ill and likely suspected or already knew that she was terminal. Why then didn’t she voice her concerns or ask questions? Who was there to support a dying woman who did not have resources? How would she have alleviation of pain and suffering —the anthem of palliative care — if she did not have a place to freely express herself? I also thought about Thambi, almost my age, doing the best he knew how for his mother. Who would offer him meaningful bereavement after his mother’s death?
I thought back to when I went through a health issue myself (by no means as serious as my patients’). Even that small disruption to my life altered my core values and left me grappling for meaning and truth. I spent hours oil painting, which is something I did as a child and had left behind in medical school. I saw a therapist, read self- help books, and learned to stare my health in the eye, with all the vulnerability and openness that requires. These skills equipped me with tools to address health-related emotion and distress.
My parents came from India so I am familiar with the culture of silent suffering. I also know that the arts are encoded in our genes. The people of India appreciate the beauty of music and the intricacies and richness of art. They practice yoga and believe in wellness derived from nature. I thought of Mrs. Kani as I started a nonprofit that trains medical staff to use expressive arts therapy for the alleviation of suffering. Expressive art therapy is not the answer — just a piece of the answer. We partner with hospitals in India that have high potential to deliver palliative care and teach their clinicians to provide quality medical care. In addition, they are trained to address the emotional, spiritual, and social suffering of the patient.
I realized quickly that when doing global health work, processes that work in one country don’t always translate into meaningful results in another. Simply having psychologists and social workers available would not help the patients because as with Mrs. Kani; there was not an acceptable way for her to engage. To bypass this barrier, our home care hospice nurses undergo training from expressive arts therapists. They are equipped with tools to meet the emotional needs of the patients in their homes. The nurses give the patients space and time to speak about their worries and fears. Often, the nurses ask that the caretakers join with the patient and engage them in an expressive art therapy activity. It seems less threatening than coming into a therapist’s office and it is more organic and natural, allowing for discussions that would not have been had without the intervention.
Mrs. Kani died a month after I saw her. I do not know if her death was painful or if she shut her eyes for the last time in peace. I do hope that the work we do, though seemingly insignificant, will allow for music and art to bring relief of suffering, that is otherwise socially denied to many of the sick and dying in India.
Preeya Desh, MD a pediatric oncologist and adult palliative care physician who founded Wabi Sabi Health to provide quality palliative care to developing countries. All names and identifying information have been modified to protect patient privacy.
Illustration by April Brust
The Dox Foundation is a 501c3 that helps clinicians reach underserved communities by funding flights for medical mission trips. To find more information and apply for your own grant, visit their website.