The progress in the treatment of T cell lymphomas was discussed in detail in this year’s SOHO meeting. Development of new treatment strategies, including cellular therapy with CAR-T cells, and finding new targets by exploring the biology of T-cell lymphomas are part of the highlights of this meeting.
CHOP-based chemotherapy is still the standard first course of therapy of peripheral T-cell lymphoma (PTCL). Dr. Neha Mehta-Shah from Washington University discussed the progress in the efficacy of the first-line treatment of PTCL by adding a medication to CHOP. The overall response to CHOP and CHOEP seen in multiple studies is approximately 75–80%. When etoposide is added to CHOP (like CHOEP), the complete remission (CR) increases from 40% to 50%, and EFS significantly improves, especially in younger patients (<60Y) and ALK (+) anaplastic large cell lymphoma (ALCL) patients.
In the randomized, double-blind, phase III ECHELON-2 trial, Brentuximab (BV)-CHP was studied against CHOP in PTCL patients where at least 10% of the lymphoma cells expressed CD30. The use of BV significantly improved PFS and OS in patients with CD30 + PTCL without increasing toxicity. BV-CHP combination has been approved by FDA for the treatment of CD30+ T cell lymphoma. The ECHELON-2 study demonstrated that biomarker-directed medication can be added to CHOP combination chemotherapy and may improve DFS and OS.
Romidepsin, belinostat, and pralatrexate are other FDA-approved medications for the treatment of PTCL. However, adding romidepsin to CHOP did not show any clinical benefits compared to CHOP in patients with PTCL. The study showed that maintaining the dose intensity of CHOP was difficult in the romidepsin-CHOP group.
Angioimmunoblastic T-cell lymphoma (AITL) has frequent genetic mutations in epigenetic modulators such as TET-2 (55-75%), IDH-2 (33%), DNMT3A (20%), RHOA (67%). The addition of the hypomethylating agent, azacitidine (CC-486), to CHOP demonstrated promising anti-tumor activity among patients with previously untreated PTCL, particularly in the T-follicular helper cell phenotype (TFH). The results of a phase II trial were recently presented at the ASH meeting. The objective response rate (ORR) was 85% after three cycles, with a 55% CR rate. At the end of six cycles of treatment, the CR rate increased to 75% for the entire cohort and was 88% among patients with PTCL-TFH. These data led to developing a new study to evaluate the efficacy of adding CC486 (oral azacitidine) or Duvelisib (PI3K inhibitor) to standard CHOP-based chemotherapy in patients with PTCL.
The non-chemotherapy, romidepsin, and lenalidomide combination was also reported at the meeting for PTCL patients who are not eligible for intensive chemotherapy, which resulted in a promising outcome with an ORR of 75%.
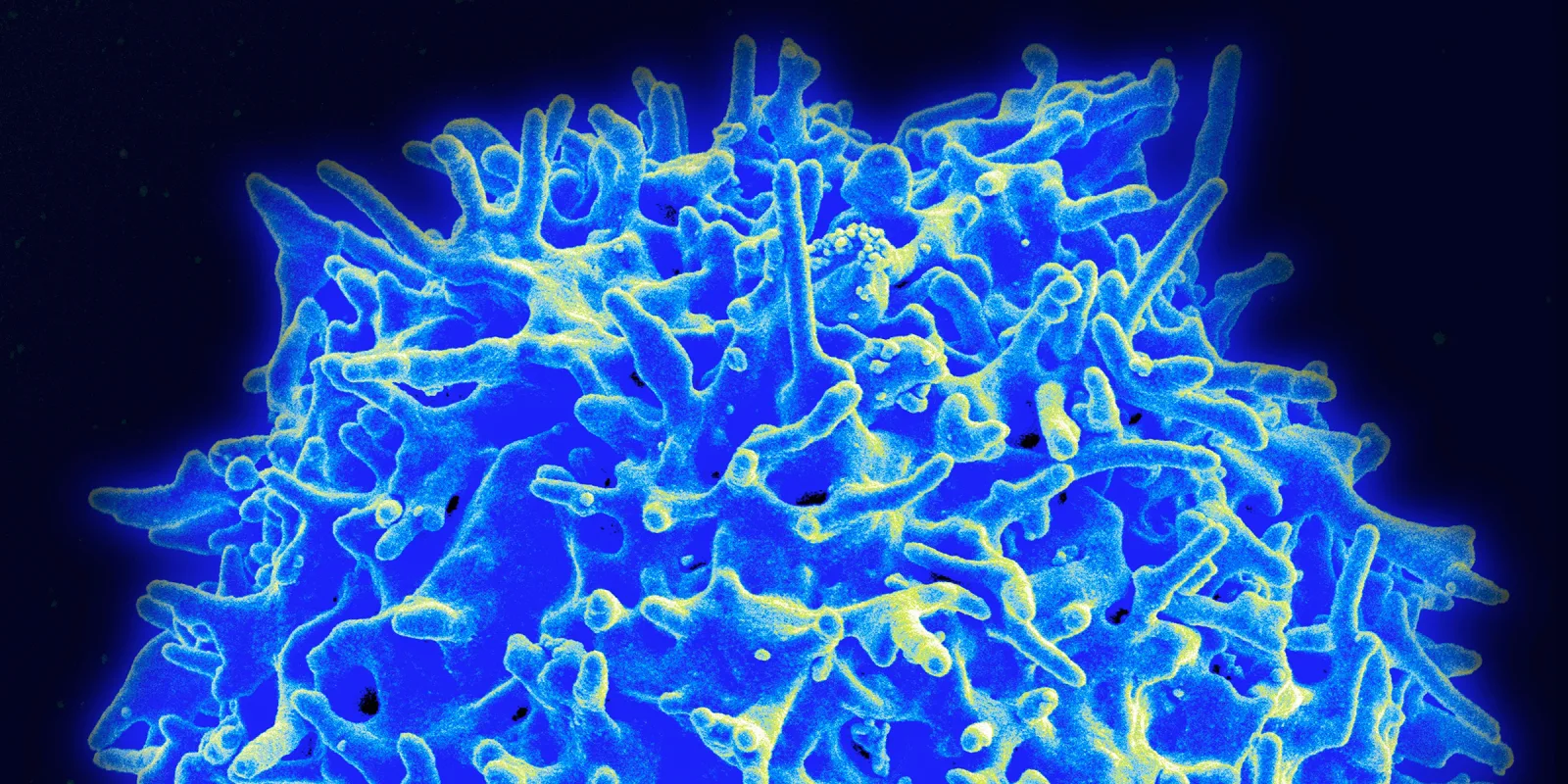
Monoclonal antibodies, including Brentuximab (anti-CD30), Mogamulizumab (anti-CCR4), and Alemtuzumab (anti-CD52), have been already used in the treatment of PTCL. Targeting the PD1 pathway has significant anti-tumor activity in patients with advanced cutaneous T-cell lymphoma. However, cellular therapy with chimeric antigen receptor (CAR) T cells has not been established yet for T cell lymphomas. The problem is that most targetable antigens are shared between normal and malignant T cells. Multiple CAR T-cell studies targeting antigens with a restricted expression such as CD30, CD4, and T-cell receptor beta chain-1 (TCRB1) are underway.
Dr. Maksim Mamonkin, from Baylor College, presented his data about the cellular therapy of T cell lymphoma. Developing CD5 CAR T cells is a novel idea, and it may be an effective strategy for the treatment of T-cell lymphomas since CD5 is highly expressed in most types of T-cell lymphomas. The targeting CD5 increases the risk of developing T-cell aplasia and fratricide of T cells. Interestingly, CD5 expression is downregulated on CD5 CAR T cells, which may prevent the fratricide of T cells. Nine patients are enrolled in the phase I study. CD5 CAR T cell infusion resulted in four (44%) responses (2 CR, 2 PR) without significant CRS and neurotoxicity. None of the patients developed T cell aplasia. Investigators recently opened a new study with CD7 CAR T cells for the treatment of T-cell lymphomas. Immunotherapy of PTCL with CAR T cells may develop a new therapy option for PTCL, especially patients with relapsed/resistant disease.
Dr. Pierluigi Porcu from Thomas Jefferson University summarized treatment options for relapsed/refractory (R/R) PTCL. The outcome of the patients with PTCL who experience relapse or disease progression is very poor. Investigators from MD Anderson Cancer Center (MDACC) reported that the overall response to second-line chemotherapy is only 44%, with a CR rate of 28%. Combination chemotherapy does not provide a better survival than new single agents. Although brentuximab in ALCL and romidepsin in T follicular helper-PTCL result in a higher efficacy as a single agent, most clinical studies showed the unmet need for better treatment of R/R PTCL. New drugs targeting specific pathways are in clinical trials, including hypomethylating agent (Azacitidine), PI3K inhibitors (Duvelisib and Copanlisib), SYK/JAK inhibitor (Cerdulatinib), anti-KIR3DL2 antibody (lacutamab), and EZH1/2 inhibitor (valemetostat). We believe that these trials will result in the development of new treatment options for R/R PTCL.
Dr. Alpdogan has no conflicts of interest to report.