There may be insufficient critical care beds and ventilators in the U.S. health care system to account for a potential tsunami of critically ill patients that will require intense, ICU-level support for many days in our hospital in the next coming weeks and months. See the most recent publication from the Society of Critical Care Medicine here. However, there will be excess OR capacity — many hospitals, as recommended by the CDC, Surgeon General, and the American College of Surgeons, are canceling all elective surgery until further notice.
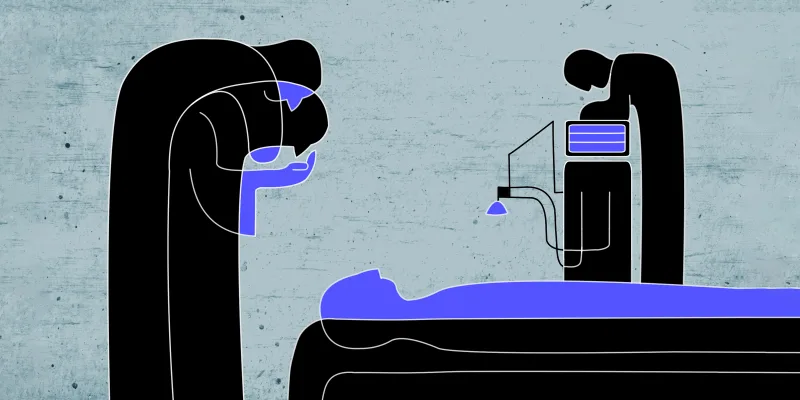
This positions ORs to become ICUs. All U.S.-based hospital ORs and ambulatory surgery center ORs have dedicated anesthesia machines which are capable for use as ventilators alone, and all the equipment that is necessary to keep critically ill patients alive is in the OR: Anesthesia machines as ventilators; infusion pumps; invasive and noninvasive monitors; equipment for IVs, airways, etc; and emergency medications.
Furthermore and more importantly, the staff in the OR are exquisitely trained to care for critically ill patients, with many providing such care daily for surgical operations on critically ill patients. The anesthesiology care is commonly led by an anesthesiologist physician who may be working alone or with physician residents, certified registered nurse anesthetists and/or anesthesiology assistants, an anesthesia technologist, a circulating nurse, and surgical scrub technologist or a surgical nurse. This team has the skills, expertise, and knowledge to care for critically ill patients in the OR.
Here's how to convert your ORs to ICUs now.
Gather Stakeholders
Affected hospitals should rapidly identify & gather relevant stakeholders in the planning and implementation of proposed changes. This can include, but is not limited to:
- Intensivist physicians; EM physicians; anesthesiology physicians
- Intensive care advanced practice providers (NPs, PAs); EM advanced practice providers (NPs, PAs)
- Physicians in training (ICU fellows and medical/surgical residents)
- ICU nurses; ER nurses; OR charge nurse
- Everyone involved in hospital administration and C-suite: Periop Medical & Nursing Executives; CMO & physician leaders; CNO & nursing leaders; CFO, finance, reimbursement from insurance & Medicare/Medicaid; COO, facilities management, systems engineering; Legal, risk management, regulatory compliance, quality & safety; Medical ethics committee, hospital patient advocate, etc; CMIO, CIO & IT for EMR & other non-PACU clinical info systems; Marketing & Internal Communications team, clinical education trainers; HR & staffing/scheduling management
Consider OR Inventory and Triage Appropriately
The OR Stakeholders (Charge Anesthesiologist, Charge Nurse, and/or Perioperative Medical Director) and COO/Facilities Management should determine the appropriate allocation of ORs: which ORs & and also an asset inventory of what equipment or capabilities are available in each OR room. Note that most ORs are NOT negative pressure rooms and thus risk the spread of airborne infection, though this is unlikely to be a significant concern given these patients are intubated.
Stakeholders should determine collaboratively the criteria for which patients to triage to the ORs for medical management. As hospitals exceed capacity, it is possible that many critically ill patients will be boarded in the ER. Criteria will need to be established that takes into consideration the different skill sets of the ER, ICU, and OR.
Considerations should include:
- Should any of the boarded ER patients be sent directly to the ORs instead of the ICU? This makes the most sense for any patients who may require surgical intervention.
- How close is the ED and ICU to the OR?
- Which patients are stable for transport?
- If an infected patient is transported, how can providers be protected?
- Can nursing ratios be changed in the ER and ICU safely so that some of the ER and ICU nurses can help with transportation and management in the Operating Rooms?
- Is an ICU-level physician available to help with the co-management of patients in the OR?
Staff Accordingly
The OR Charge Staff (Charge Nurse & Physician Anesthesiologist) will have to determine what sort of staffing ratio will be appropriate for the transferred critically-ill patients. Typically anesthesia-level care in the OR requires an anesthesia provider at all times. However, given that this is critical care rather than anesthesia care, it should be possible to staff these patients in a similar fashion to the critical care units, with single physician anesthesiologists supervising care in ICU ratios of 10:1 or more patients to a physician, while understanding that given these patients may be among the most critically ill while being cared for in a non-ICU setting, situations may require 1:1 staffing of providers and nurses. Centralized data exchange will facilitate care for multiple critically ill patients in the OR. For example, the circulating nurse could stay in the OR with the patient, checking ABGs and labs, making changes to the ventilator as directed by the supervising anesthesiologist. The supervising anesthesiologist can monitor multiple patients from a centralized location in the hospital. Residents, CRNAS, and anesthesiology assistants can provide 1:1 bedside care when it is required. Respiratory therapists can also be shared among many ORs to aid in suctioning patients and changing positions if it is required (prone positioning for ARDS, etc.) And because these patients will require 24-hour care, staff will have to be rotated on an 8 or 12-hour basis, with standard built-in breaks to ensure optimal care.
Facilities management and other staff need to ready those OR rooms by placing signage in the appropriate places that notes patient is a critically ill medical patient; making sure the rooms are removed from the OR scheduling system; removing the OR bed from the room and any surgical equipment that can potentially be contaminated; finding ICU and/or Med-Surg beds for long term management of ICU patients in the OR.
Communicate Efficiently
Once the above steps have been completed, a single point of contact from the ICU (likely the physician intensivist) and a single point of contact from the OR (likely the physician anesthesiologist) should coordinate the care of the patients being transported from the ER or ICU to the OR. This includes the clinical handoff/sign out of all relevant info, communicating vents/lines/tube information, confirming if any drips need to be prepared, and what the clinical criteria is for when a patient receiving ICU-like care in an OR would need to be brought back to the ICU?
Please share this with your hospital leadership and colleagues to start the conversation and conversion.
Image: OxfordSquare / shutterstock
Click here to see more perspectives on COVID-19 from the Doximity network.
Click here for up-to-date news about COVID-19 on Doximity.