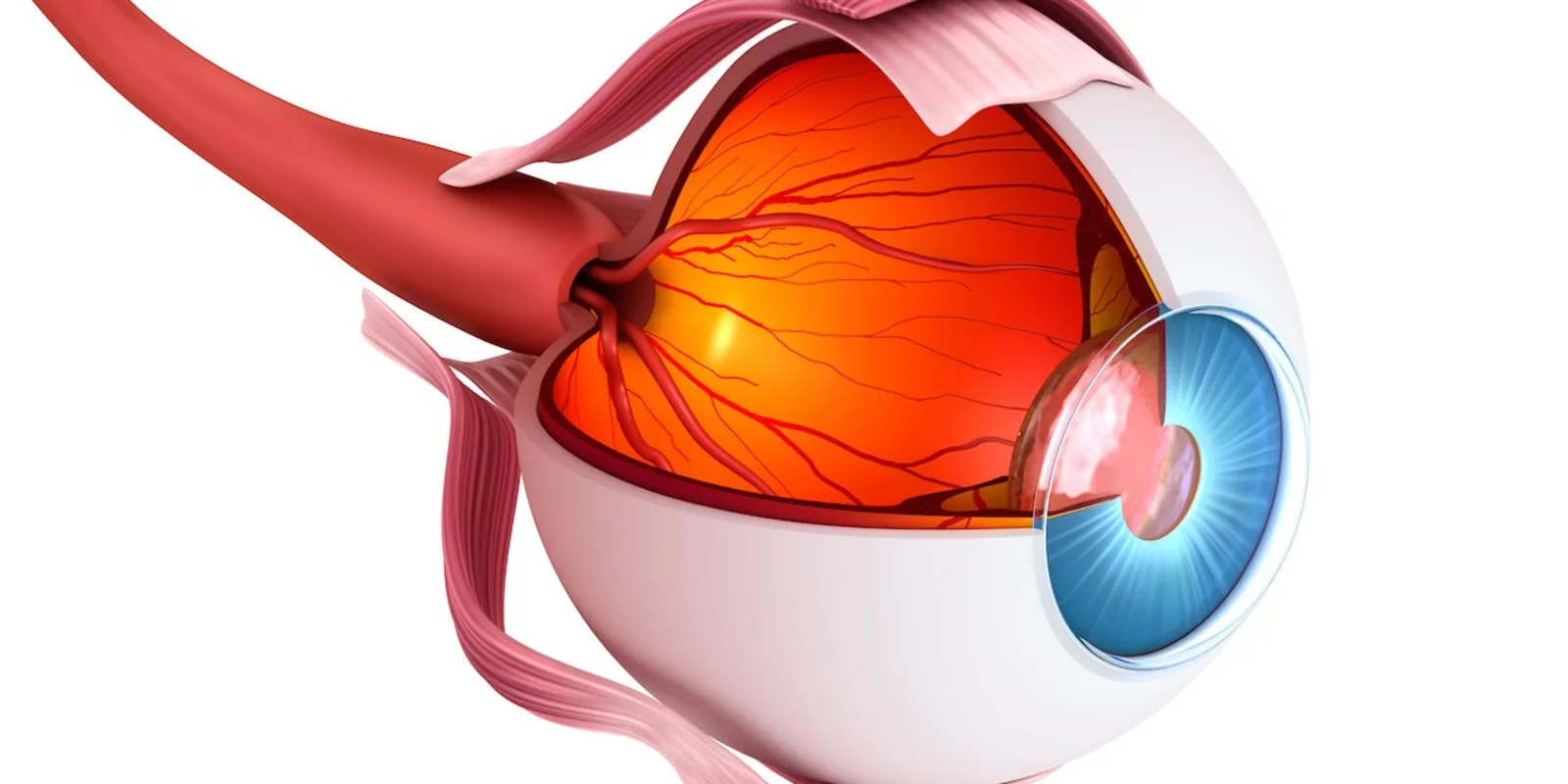
Macular holes result in permanent loss of central vision in the affected eye unless the hole is repaired. Closure of macular holes, however, can result in restoration of very good vision.
Prior to vitrectomy, macular holes were largely untreatable. With the advent of vitrectomy—separation of the hyaloid vitreous from the retina and placement of a gas bubble with face down positioning—resulted in hole closure in nearly 9 out of 10 cases.
The addition of internal limiting membrane peeling has led to nearly 95% hole closure rates. At the recent annual meeting for the American Society if Retina Specialists in Vancouver, Canada, retina specialists had gathered from around the globe to evaluate novel approaches to large or chronic holes that often don’t close up.
The placement of inverted flaps over macular holes is established and largely accepted. However, Dr. Srinivas Joshi reported success with a unique petalloid flap placement technique in 45 eyes with large holes. Further, Dr. Naresh Kannan presented a comparison between inverted ILM flap repair and the placement of platelet-enriched-plasma in the hole. In their hands 86.7% ILM flap vs. 93.3% platelet-enriched plasma closure rates occurred in these difficult cases.
Dr. Kazuaki Kadonosono presented new data on autologous neurosensory retinal graft placement in refractory macular holes. The technique is still investigational to the audience but anatomic closure occurred in 89.8% of holes with vision improving in 42.8% of holes. Along the lines of tissue patch placement Dr. Stanislao Rizzo presented preliminary success with placement of a biocompatible film to promote macular hole closure and described his technique for graft placement.
Further, Dr. Christian Pruente has identified a ring of material in persistent macular holes that he lyses with three radial incisions. He reports an 80% success rate with this technique and despite cuts into the macula edge there is a mean gain of three lines of vision.
In trying to make macular hole surgery easier for patients, Dr. Raymond Lezzi reported on 18 eyes with chronic and large macular holes that underwent ILM peel and placement of C3F8 gas and modified positioning instructions, including not sleeping on their back and no true face down positioning. He reports that 83.3% of these holes closed in a single surgery.
Potentially improving patient experience further, Dr. Calvin Mein reports 2-center experience with pneumatic vitreolysis on treatment of focal vitreomacular traction 85.5% success rate, and stage 2 macular holes 61.9% success without vitrectomy surgery. This inexpensive and office based procedure is of significant interest and is pending further evaluation.
In summary, the profession presented significant innovation and progress in managing the most difficult macular holes at the meeting. They are also improving patient comfort and reducing cost in managing those holes most likely to close successfully.
Dr. Peter L. Gehlbach is a professor of Ophthalmology at the Wilmer Eye Institute, Johns Hopkins University School of Medicine and the Whiting School of Engineering. A former director of retina training at Wilmer, he is now an active clinician-scientist and teacher in retinal microsurgery.