Postpartum psychosis (PPP) is a rare and severe disorder considered a psychiatric emergency. But it remains the subject of controversy as a diagnosis in the DSM V. Yet PPP is the only mental illness consistently associated with a homicide (infanticide) rate of 4%. Perinatal suicide is the leading cause of maternal death (20%) in the first postpartum year. Women with PPP have the highest suicide risk at 5%, with violent methods such as hanging and jumping. Only 3% die from an overdose. Despite this mortality rate, it is not a formal diagnosis in the DSM V.
PPP was included in the DSM I as Involutional Psychotic Reaction and DSMII as Psychosis with Childbirth. PPP was erased from the DSM III and DSM III-R, which covered a period of 14 years, from 1980–1994. When “postpartum” was expunged from the DSM, a generation of American psychiatrists and physicians in training abandoned the existence of mental illness associated with childbearing.
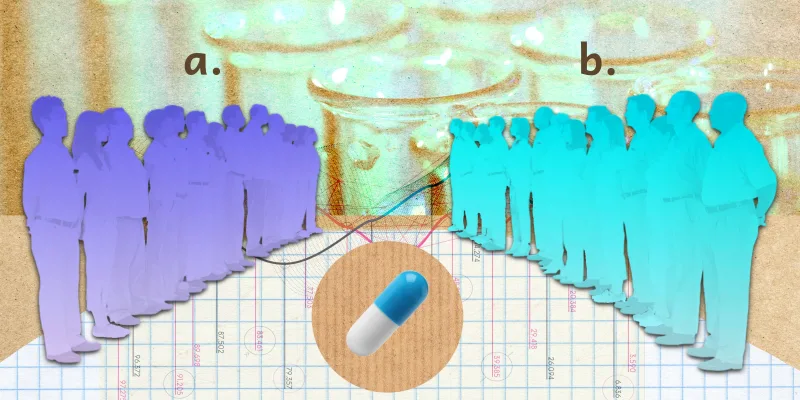
The rate of PPP is 1-2/1000 in the general population. However, bipolar women with a family history of bipolar disorder have a 30% chance of having a PPP and a 70% chance if they have a first-degree relative with PPP.
Mothers suffering from this mental illness can experience hallucinations that may take the form of commanding voices, bizarre delusions, racing thoughts, insomnia, mood lability, perplexity, and confusion. Most significantly, PPP is frequently accompanied by a delirium-like state, which distorts the mother’s judgment. While in the grips of psychosis, some mothers have become so dominated by uncontrollable thoughts that they have killed their infants. A psychotic mother must be immediately hospitalized and separated from her infant.
In the U.S., a postpartum woman who kills an infant during a psychotic episode is arrested, charged with homicide, and incarcerated. Punishments are often severe such as life sentences and even the death penalty. Recently, a 23-year-old California mother who killed her three infants received three life sentences.
The U.K., Australia, Canada, and 21 European countries, aware of these facts, have Infanticide laws for women who kill a child in the first year of life. Based on the biological vulnerability of childbirth, women found mentally ill receive psychiatric hospitalization, not punishment. And yet, the U.S. has the highest infanticide rate of all western countries (8/100,000; Canada 2.9/100,000; Italy 2.7/100,000; New Zealand 4.5/100,000).
The clinical utility of a formal diagnosis for PPP includes proper symptom identification for diagnosis, treatment, prophylaxis, and protection of mother and infant. In the absence of a formal classification of PPP, and to assist clinical decision-makers, we overlook psychotic women leaving them and their infants in danger.
The lack of a DSM diagnosis makes it difficult to assert an insanity defense in cases of infanticide. In asserting an insanity defense based on postpartum illness, a defense attorney must have two types of evidence: a documented diagnosis of a mental illness and evidence of a woman’s behavior before and after the crime demonstrating an inability to form specific intent. Although the current nosology includes “postpartum onset” as a “specifier” to a diagnosis, it is not a specific, identifiable diagnosis with characteristic symptoms and behavior, which are necessary to support a defense of insanity.
The DSM flies in the face of biology. It disregards the neurohormonal triggering factors of childbirth and the impact of hormone changes on the brain. This field has developed in parallel with the discipline of neuroendocrinology, a science that studies the profound effects of hormones on brain chemistry and subsequent mental illnesses that occur from these effects. Parallel changes in the immune system and analogous genetic vulnerabilities in these women support the biological foundation of PPP.
PPP has a unique picture that fulfills criteria (impaired cognition, emotional dysregulation, and behavior symptoms) for a mental illness as suggested by the DSMV. In the absence of formal DSMV diagnosis do American psychiatrists fail to identify and properly treat postpartum psychosis keeping our infanticide rates soaring above those in other countries?
Dr. Spinelli is employed by Columbia University College of Physicians and Surgeons and has no conflicts of interest to report.
Image: goodstudio / shutterstock