Everyone seems to want to make patients better consumers. The underlying hypothesis is that if we educate patients with dismally low health and insurance IQs, then they will become more engaged, which theoretically would give them the incentives to change their consumer and health habits, which would bend the cost curve.
However, those are a lot of assumptions and, unfortunately, research suggests they are not valid.
Patient engagement does not necessarily mean patient activation, which has been correlated with better outcomes for less cost.
Personalized learning has won favor with Silicon Valley types because it blends traditional education with cutting-edge technology. Schools often use both hardware and software to help kids learn at their own pace and in the style they most prefer. On average, personalized learning led to 130 percent growth in reading and 122 percent growth in math.
Patients need to raise their IQs in three major areas: health systems, insurance, and patients' own illnesses.
The Institute of Medicine defines health literacy as the degree to which individuals have the capacity to obtain, process, and understand basic information and services needed to make appropriate decisions regarding health. Health literacy in patients with head and neck cancer, for example, can be measured using general and specific tools, which identify gaps in education and understanding.
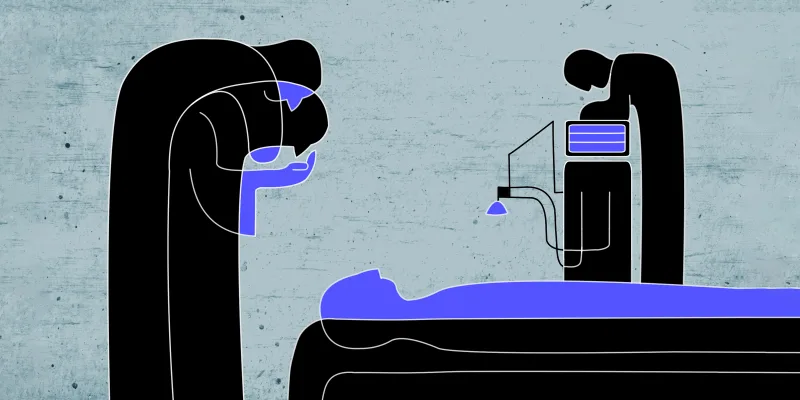
Fundamentally, doctors are teachers. So, it is not unreasonable to propose that patients should fundamentally be students.
So, how would we approach patient engagement strategies if the goal is to increase patient grades?
Here is the website for the Denver Public Schools student portal. Notice:
- 1. Parents can sign in to see how their kids are doing. Caregivers should be able to do the same.
- Student grades are posted. We are very willing to post grades for doctors—why aren't we doing the same for patients who are not doing their assignments?
- Disciplinary notices are posted. Why don't we do the same for opioid abusers and flagrant abusers of the sick care system?
- The portal has videos on how to use it (i.e., the portal) to improve performance. Why don't we do the same with patient-students?
- The portal posts academic standards and compares student performance. We should do the same for patients, and compare them to how other patients are doing with the same diseases.
- Students have incentives to do homework. We should have patients send in progress reports using patient-reported outcomes technologies.
- School systems have parent-teacher nights. We should have nights for family members and caregivers.
- Students have recesses. We should have opportunities to provide patients with a sense of community to fight loneliness.
- Students have access to school nurses—patients should be able to access alternative providers.
- Students have access to school psychologists to manage behavioral health issues—so should patients.
Personalized patient and doctor learning is driven by technology, learning theory, and data analytics. Since there are multiple learning styles, one size will not fit all—nor should we expect it to when it comes to changing patient and doctor behavior.
Patients only remember about 49 percent of the information their doctors give them without prompting,which highlights shortcomings with patient recall that can negatively impact patient activation (see this study out of Brown University School of Professional Studies). But we need to take patient education and learning much further than just recall. We need to get to interpretation (i.e., what does this information mean?) and problem solving (i.e., what should I do next?)
Informed consent is not the same thing as patient understanding.
Raising patient grades means treating them like students first. Nobody flunks—but they might have to repeat a few grades until they get the right answers.
Arlen Meyers, MD, MBA is the President and CEO of the Society of Physician Entrepreneurs.