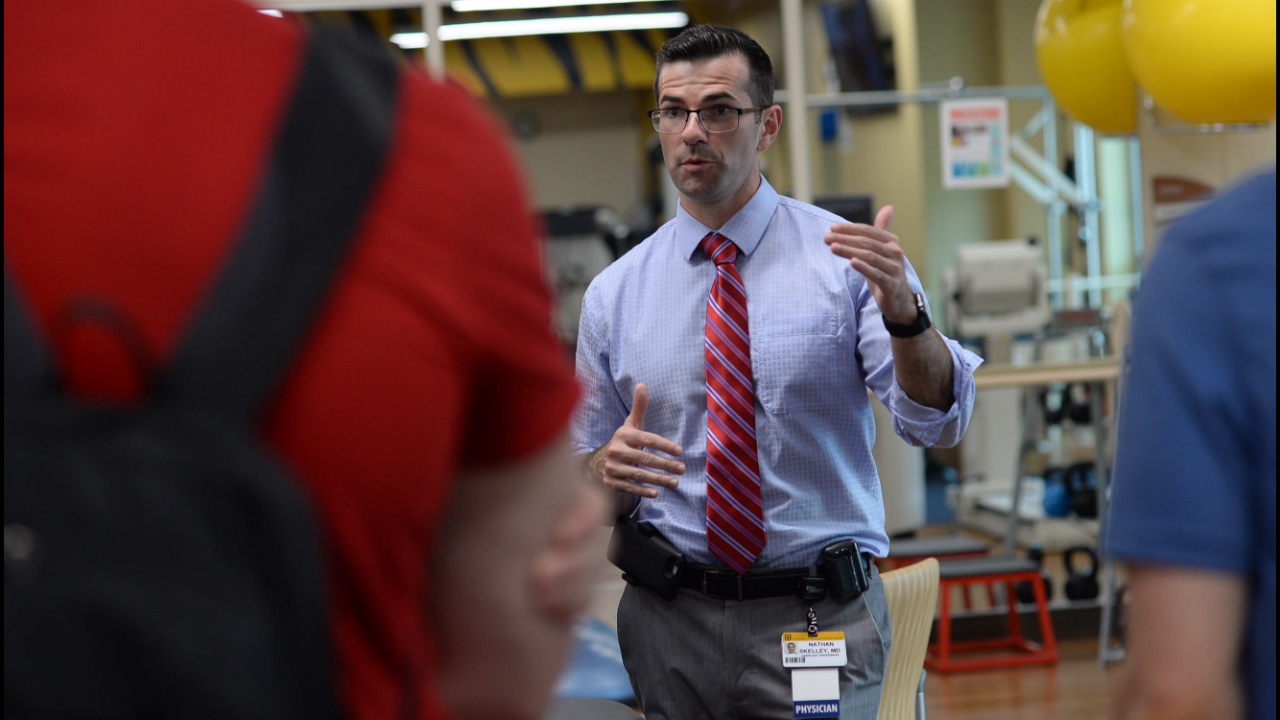
Name: Nathan Skelley, MD
Specialty: Orthopaedic Surgery
Education: Harvard Medical School, Washington University in St. Louis, Johns Hopkins University School of Medicine, Cornell University
Areas of Expertise: Sports Medicine; Shoulder, Elbow, Hip, Knee, Foot and Ankle Surgery
Current Position: Assistant Professor of Orthopaedic Surgery, Missouri Orthopaedic Institute at the University of Missouri
1. Why did you choose orthopaedic surgery?
I grew up in a medical family — both of my parents were involved in medical fields. Additionally, my first occupation was teaching Sho-Tae-Ryu martial arts. I earned the rank of black belt first degree under the instruction of Master Billy Moody. I enjoyed learning how the musculoskeletal system functioned, and I carried this passion throughout my education and medical exposure. This experience had an important impact on my path to a career as a sports medicine orthopaedic surgeon.
2. What area of orthopaedic surgery is changing most rapidly?
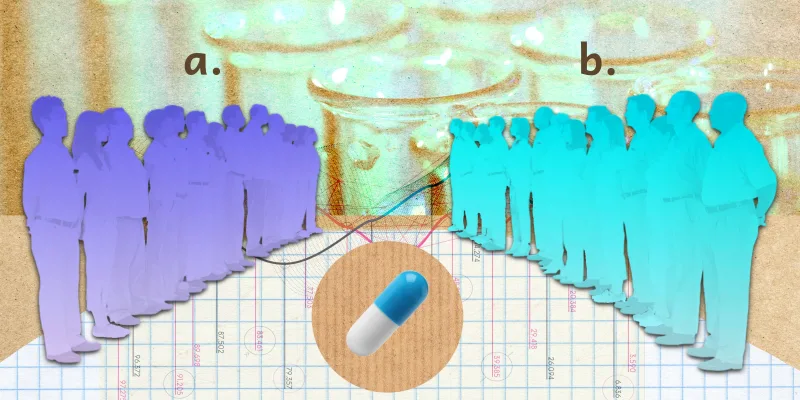
The field of orthopaedics is closely associated with many emerging technologies. There are many exciting and rapid developments in our field. Orthobiologics is an area of sports medicine that is rapidly developing and becoming more important in treating patients. 3-D modeling, orthopaedic simulation, and mobile technologies are also improving and changing the field.
3. What are your research interests?
My research is focused on emerging technologies in orthopaedics. I have a great interest in 3-D printing technologies and their role in improving orthopaedic care in rural areas. I also enjoy studying mobile technologies and biosynthetic grafts. I hope by the end of my career, sports orthopaedic surgeons have a good alternative for grafts instead of taking autografts for reconstructive procedures.
4. What are you learning now? Why is that important?
I am learning to perform CAD file creation and manipulation to make 3-D printed implants and also segmentation protocols to 3-D print orthopaedic models for preoperative planning, simulation, and treatment modifications.
5. What is a common misconception that other clinicians or the general public have about your specialty?
I think many other specialties see orthopaedic surgeons as very focused on, “Bone broke, me fix.” But that’s only part of what we do every day. Orthopaedic surgery has developed into a very complex specialty with numerous sub-specialties. For a medical student to say they want to go into orthopaedic surgery, is somewhat similar to a student saying they want to go into medicine and then later sub-specialize. Orthopaedic sports surgeons have very unique and different practices compared to orthopaedic spine, arthroplasty, shoulder/elbow, foot & ankle, etc. surgeons.
6. Who are your mentors?
My greatest clinical and professional mentors have been my parents, Mark and Billie Skelley. They both worked in medical fields and taught me about the impact a physician can have on the life and quality of life of a patient. During my time at Johns Hopkins University, Carl A. Johnson, Edward McFarland, and Paul Sponseller were extremely important to my development and interest in orthopaedic surgery. As an orthopaedic surgery resident, Jay Keener, Robert Brophy, and Matthew V. Smith were very important in helping me decide on a specialty focus in sports medicine. During my fellowship, Scott Martin, Luke Oh, Jon Warner, and Eric Berkson helped me focus my skills and practice into what they are today. I believe physicians are always learning and will always have mentors and mentees. Even as an attending physician, I am thankful for the mentorship of my colleagues Matthew J. Smith, Benjamin Summerhays, Shen-Ying (Richard) Ma, and James Stannard.
7. What is the best advice you have ever received?
The best advice I ever received was from my grandfather Paul B. Skelley, M.D. He was a general surgeon and served in WWII. I don’t know if it’s because I complained a lot as a child or if he just noticed I was taking on many different challenges throughout my education and training but he would frequently tell me, “No one said it would be easy.” To this day, when my research is not working out the way I anticipated or when I get a complicated referral from an outside hospital, I think, “No one said it would be easy,” and I get back to the challenge at hand. I am forever thankful to my grandfather for teaching me this lesson and giving me this advice.
8. What has been your most gratifying moment of being a clinician?
The most gratifying moment of being a clinician is when I’m able to restore a patient to their previous level of function or ease their pain. To help them get even better function than they had before their injury or condition is also a very rewarding feeling. It means a lot to see a patient succeed and appreciate the time and expert specialty care we provided to get them back to work or back in the game.
9. I start each day by telling myself…
“Get… out… of… bed…” I think the first step is many times the most challenging, but if you can get past that, there are endless opportunities.
10. How do you unwind after a challenging day?
Sleep.
11. How do you motivate your patients to do what’s best for their health?
Education and communication are key in my experience. If I am able to clearly communicate their situation and help them understand the consequences of their actions they can take the necessary steps to create change in their healthcare. Although I have no data to support this, I have been surprised how many of my patients are able to lose weight or stop smoking before a surgical procedure. I think it is because we take the time to talk about these issues and how they impact their musculoskeletal care. Similarly, we develop plans and strategies to correct these issues before proceeding with surgery to give them the best possible outcome.
12. When in your career did you feel most despondent and what did you do to turn it around?
I think it is possible to feel despondent every day in medicine. Clinicians are supposed to cure disease and end suffering — those are very daunting tasks. Add on top of that administrative hurdles, a complicated insurance system, physician debt, and an unhealthy medico-legal climate and it’s not hard to understand the high rates of physician burnout. I try to focus on the positives in my everyday practice and adapt to the daily challenges. Bruce Lee had a great philosophic thought when he said, “Be like water my friend.” I try to be like water as well in my medical practice.
13. Do you do anything special or have any unique hobbies or interests?
During my fellowship in Boston, one of the faculty, Dr. Eric Berkson, challenged the fellows to learn a skill completely unrelated to orthopaedic surgery during their fellowship. I came from Missouri, a land-locked state, and had never sailed in my life. Sailing is a very popular hobby throughout New England. On top of my fellowship duties, I became a fairly competent Cape Cod Mercury sailor and still enjoy the hobby today on lakes in Missouri.
14. What are your favorite Doximity features and how have they helped your productivity? (Dialer, DocNews, Career Navigator, e-Fax, etc.)?
The Doximity Dialer is the best tool I use in my clinical practice. I have told several of my colleagues about the app and they all enjoy using it. It is a great way to stay in contact with my patients without having the patients use my personal cell phone.