There are more than 600,000 people in the United States living with end-stage renal disease (ESRD). With a wholly inadequate supply of kidneys to transplant, ESRD patients have to filter metabolic waste and extra fluid out of their bodies in order to survive. The vast majority of ESRD patients (~90%) choose hemodialysis (HD) over peritoneal dialysis (PD) to accomplish this process.
Why choose HD when PD has better outcomes and saves money? After all, ESRD is one of only two specific diseases that Congress has enacted law to specifically cover, regardless of a patient’s age (the other is ALS). As a taxpayer, I vote for providing optimal treatment — that backed by the weight of medical science — especially when it’s the more cost-effective option.
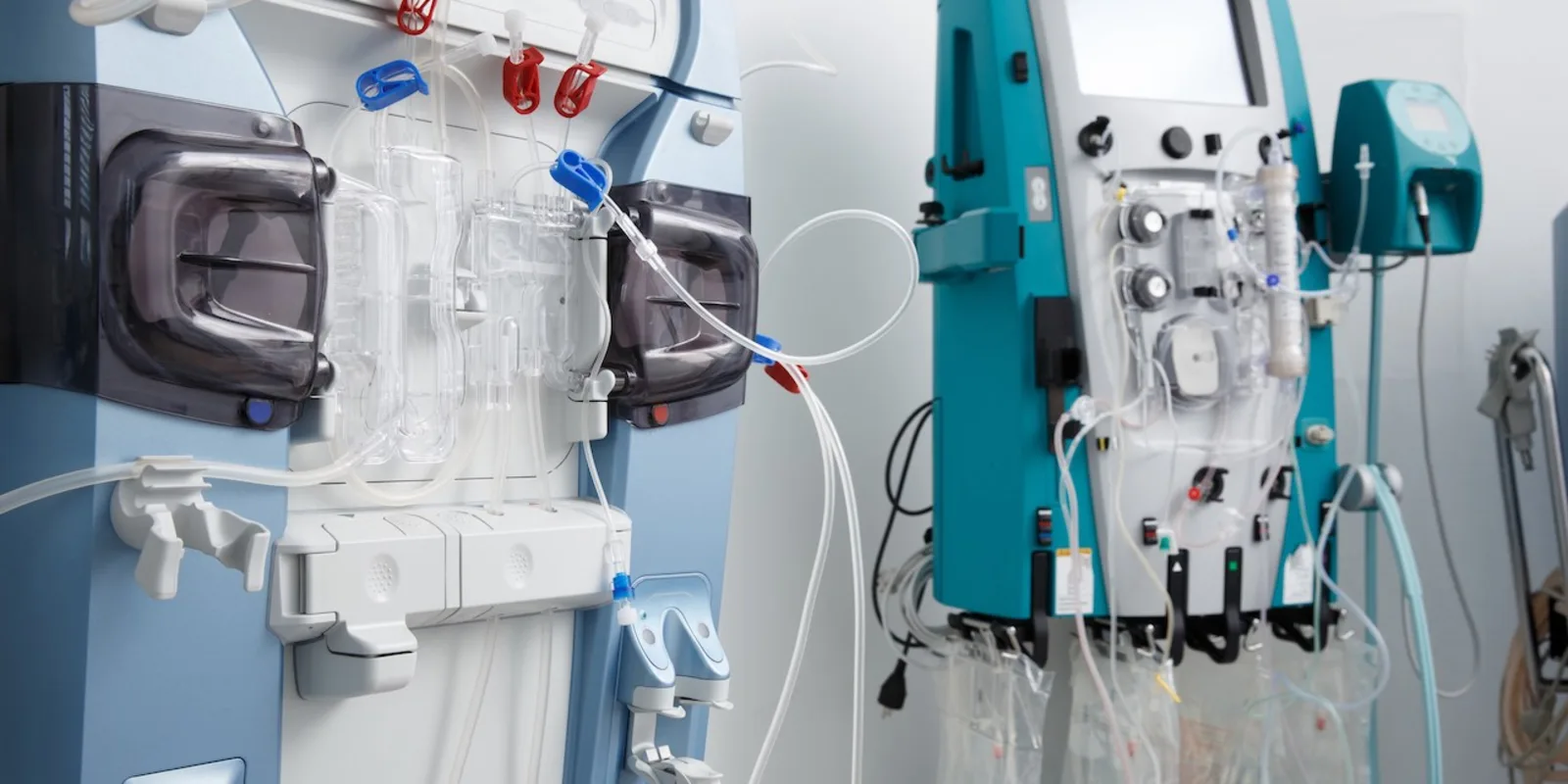
In conventional HD, patients travel to a dialysis center three times a week and plug in to a dialyzer for three to four hour sessions to have their blood filtered. Thrice-weekly sessions make it nearly impossible to engage in full-time employment, and patients often suffer during dialysis sessions with nausea, muscle cramps and itching, to name but a few side effects.
In PD, patients can self-administer their dialysate through a catheter in their abdominal wall and cycle through fluid nocturnally, even while they sleep. The patient’s own peritoneal membrane handles the diffusion. How brilliant is that?
Home convenience makes PD less disruptive to a patient’s lifestyle, and full-time employment can be more easily maintained. In addition, dialysis side effects are mitigated as PD sessions run longer in duration. The overall cost of PD administration is lower, and since PD patients have fewer hospitalizations, the aggregate cost for this group winds up being about 15% lower per capita than for patients who choose HD. Best of all, patients on PD have fewer complications and live longer.
So why are only 10% of ESRD patients choosing PD? Survey data shows that when provided adequate information, the PD rate could be somewhere closer to 40%, which would lead to significant decreases in morbidity, mortality and cost.
Jake Harper of Side Effects Public Media recently reported on the large gap between HD and PD, and some of the reasons why it’s still so large. Hint: follow the money.
After Congress legislated Medicare coverage for ESRD in 1972, the next decades saw a profusion of outpatient dialysis centers open, as there would always be a steady stream of ‘customers.’ For one thing, the U.S. population invariably grows, which means even at a steady state of ESRD, more people need dialysis every year. And with Medicare covering all charges for ESRD patients, a payor source is thereby guaranteed. Enter doctors, hospitals, and eventually, investor-owned companies into the fray. Dialysis is big business.
According the latest full year of data from the U.S. Renal Data Service, Medicare paid $34 billion in dialysis-related costs. Though only 1% of Medicare patients are on dialysis, the practice consumes 7% of the program’s total expenditure. So something is out of whack.
For much of the dialysis era, hemodialysis was billable at higher rates — this was true of the service itself and the physician fees associated with evaluation and management. With numerous centers around the country, nephrologists and their teams could see dialysis patients in bulk fashion since their patients were literally tied to their dialysis chairs three times a week. Thus, it’s no surprise that HD dominated the market.
According to many in the field, the dominance of HD led to further diminishment of PD because of the cultural preference for HD on the part of both doctors and patients. In the early 2000s, PD rates fell as it was even less appreciated as a viable alternative to HD.
Fortunately, changes to reimbursement over the last several years have moved incentives in the other direction, as it’s become more clear from the medical evidence that PD is just as good (many studies prove superior) to HD. It’s no longer more lucrative from a billing standpoint to offer HD versus PD. Even more encouraging is news that the two largest providers of dialysis services in the United States, DaVita and Fresenius (both publicly-traded conglomerates which together control 70% of the market) are amping up their PD services and encouraging more widespread use.
One barrier to wider adoption of PD is that it’s still more convenient for doctors to see patients in higher volume at dialysis centers. Nevertheless, I’d expect to see a doubling of PD rates in the next decade now that incentives have become better aligned.
Medicare: We may not always get it right the first few decades. But if we learn to trust the science and implement sound policy, there’s no reason we can’t become both more patient-centric and cost effective.
Dr. John Henning Schumann is an internist and a 2018–2019 Doximity Author.