As I enter the exam room, my eyes are drawn to a small mask covering a large beard. I can almost see the large respiratory droplets escaping through the gray hairs. It’s quickly apparent that my patient's speech impairment is much more severe than his chart indicated. Frustrated that I am not aware of this, he gestures and grunts loudly. Soon, he is within inches of my face as his loosely fitted mask falls below his mouth. I’m grateful for my face shield blocking the invisible yet large respiratory secretions projected my way. I wondered — however — if my surgical mask would block the smaller, aerosolized ones propelled into the air by his forceful grunting?
When the summer surge was beginning to take shape in June, the Lancet published a meta-analysis on PPE and physical distancing measures, concisely summarized by The New York Times. They found that surgical masks reduced the risk of infection by 67%. N95 masks, on the other hand, boasted 96% protection.
By the time we bid good riddance to 2020, millions of front-line health care workers are expected to receive their first doses of a highly efficacious and safe COVID-19 vaccine. After their second dose just weeks later, they will be approximately 95% less likely to develop symptomatic COVID-19. In the meantime, why would we ignore the remarkable efficacy of N95 masks?
As the winter tsunami grows, we should no longer withhold N95 masks from health care workers in higher-risk scenarios where proper distancing can’t be maintained, and the quality of patient PPE is difficult to regulate. Yes, some health systems still report shortages of N95 masks. Yet, many are well-equipped. In California, where I practice internal medicine, my colleagues across the state report sufficient N95 supplies, even as we currently lead the country in COVID-19 hospitalizations. Gavin Newsom, California’s Democratic governor, signed a law that all hospitals are required to have three months of PPE on hand. Governor Newsom also frequently highlights that the state’s stockpile has over 178 million N95 masks, which are in addition to the large stockpiles managed by health systems throughout the state.
There are likely more than enough N95 masks throughout the country to last until the majority of health care workers are fully immunized. Those in short supply could purchase more N95 masks in the interim, which would be less costly than health care workers falling ill. Many want to wear their privately purchased N95 masks in routine patient care settings but are strictly forbidden by their hospital or clinic from wearing anything other than the loosely-fitted surgical mask provided to them. Some of these workers have now contracted COVID-19 on the job, despite adherence to PPE protocols. The risk may be greatest not in the ICU, but rather in primary care and other outpatient settings, where robust PPE is less widely available and where patients are more likely to be seen when asymptomatic or mildly ill, yet are paradoxically most infectious. With rising rates of infections among health care workers and more patients in need of their care, they must be better protected.
In places where the top-of-the-line N95 masks are scarce, we have other options much better than surgical masks for those at higher risk of exposure to COVID-19. Studies have shown that most N95 masks can maintain excellent filtration if used for up to two shifts; use beyond two shifts is likely much better than a surgical mask. N95 masks can also be safely sterilized for reuse. Would I want to don a reused N95 mask while intubating a COVID-19 patient? Not ideally, but against the backdrop of widespread community transmission, I would certainly choose it over a surgical mask, especially when examining vulnerable patients in a small exam room or when shoulder-to-shoulder with other health care providers in confined workspaces. And with growing evidence that fewer viral particles inhaled may result in a lower risk of symptomatic illness, we must do all we can to limit exposure.
As the winter surge accelerates, health care workers are exhausted. We’re just weeks away from reaping the fruit of scientific ingenuity and capital investments that have produced a remarkably effective and safe vaccine. On the cusp of victory, we want to be fully protected so we can fight back the final surge of this once-in-a-century pandemic. We should double down on the effective PPE at our fingertips and allow our most vulnerable health care workers to protect themselves from infection while they protect others. When this pandemic is over, let’s not look back at our large piles of excess N95 masks and regret withholding them from our health care heroes in their hour of greatest need.
Do you have enough protective equipment? Let us know below.
Kenny Pettersen, MD, MPH is a general internist practicing in Los Angeles, CA, and dedicated to fighting health inequality in resource-poor settings.
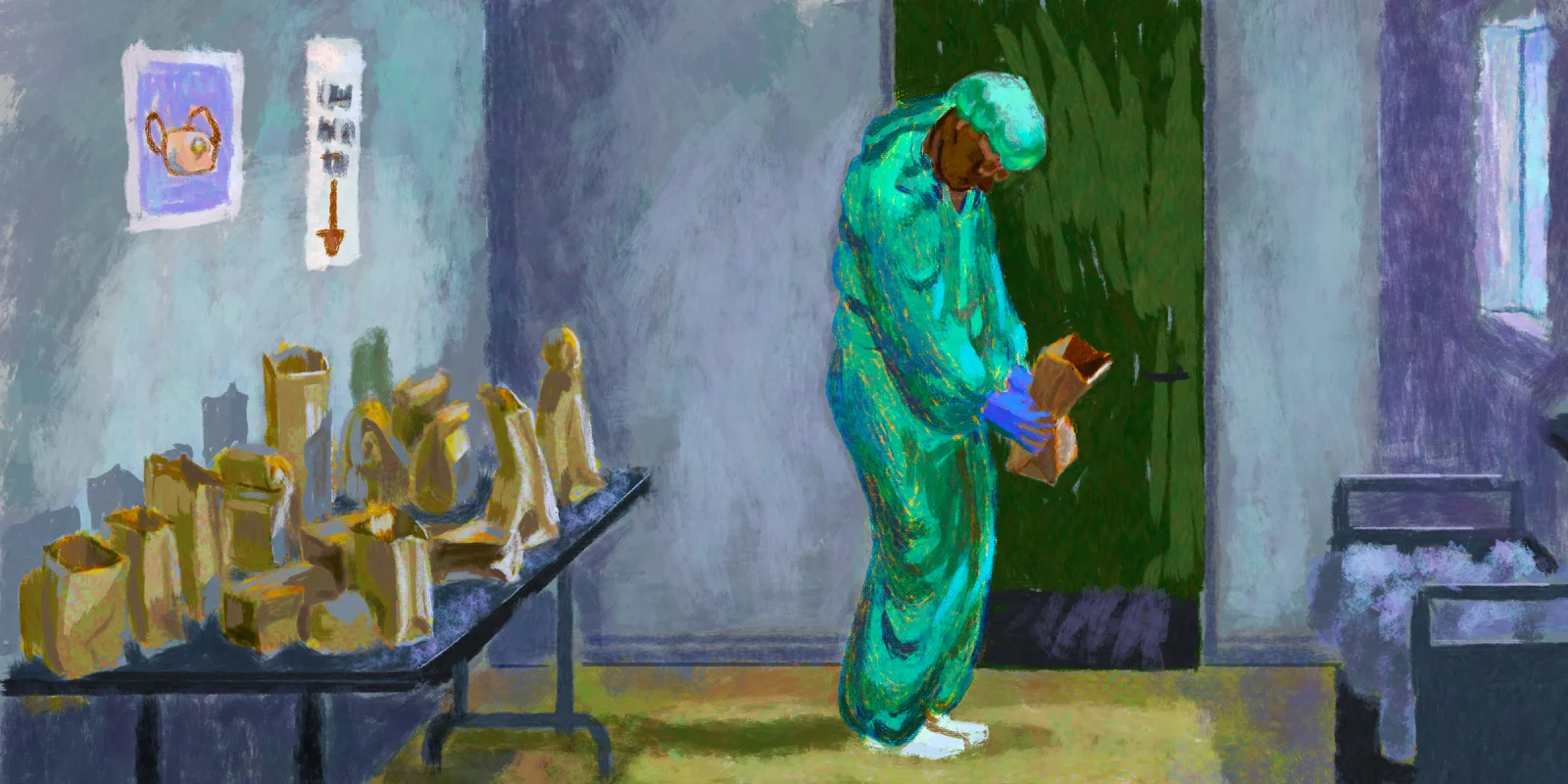
Illustration by Jennifer Bogartz
Click here to see more perspectives on COVID-19 from the Doximity network.