The words were like bitter candies that I had been sucking on, hoping to come to a sweet center. I had walked the hallways of the hospital holding them in the silky pocket of my cheek for weeks. Finally, afraid I would choke, I spit them out into the middle of the dinner table.
“I think I’m depressed.”
I stared down at the tablecloth, moisture collecting on the base of my water glass. My hand shook as I raised the glass to my mouth. Droplets spattered onto my bare leg and I smeared them with a palm already damp with tears. A hand reached for mine and as I raised my eyes, I looked around the table to see my colleagues nodding, eyes brimming with emotion. Were we all in the same boat? It felt like it was dangerously close to sinking.
It was about six months into my intern year and I was sitting around a table with a handful of colleagues. I had heard that winter of intern year was supposedly the most difficult — the darkness of the days was amplified by the length of hours we spent at the hospital. But the darkness outside had started to seep into me, and I was starting to get worried.
I had recently worked on Christmas Eve, a holiday usually full of joy and celebration. This year, away from my family, I had clipped three pagers to my hospital scrubs and carried around an energy drink while I admired the hospital Christmas decorations in between admissions and thankless tasks. The following morning, I delayed leaving the hospital because I knew I’d be going home to an empty apartment. Later, I lay on the floor in front of my heater, too tired to turn the lights on. I wondered what would happen if I didn’t show up to work the next day — or the day after that. Then, I put on a smile to Skype with my family, and fell asleep still wearing my scrubs.
Now, as the conversation wound its way around the table, I discovered that the feeling of isolation and despair reached out and wrapped its tendrils around my colleagues, their spouses, and even their families as well. We discussed the fatigue, the stress, the high-stakes decision making we were learning to deal with. We touched on our concerns over our emotional and physical health. We threw all of our concerns into the middle of the table and as the pile grew, the weight on our shoulders lessened.
As we left the restaurant that evening we left Shame behind, sitting at the table alone, and made a pact to watch out for each other for the remainder of our time together — both in residency and beyond. My connection with these six people served as a foundation of unwavering support during my years in residency. I’m happy to say it still exists for me today, and it still serves a purpose even beyond the stress-filled years of residency and fellowship.
I often wonder what would have happened in the absence of that dinner conversation. If we would have stayed silent, each in our silos of sadness, would our career paths have been cut short? It’s not an unreasonable question.
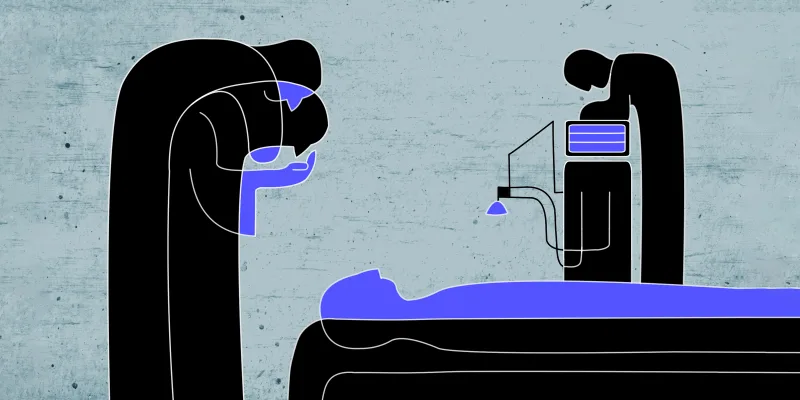
In the wake of yet another medical student who took her life too soon, we have to wonder why the support of our students and physicians-in-training is typically stunted. If you consider that medical providers hold a suicide rate higher than the general population (and young physicians among the highest), it’s obscene that physician mental health, and suicide in particular, tends to remain a taboo topic in most institutions.
It is well-known that major trauma lends itself to changes in the brain that can be emotionally debilitating. It is no surprise then, that the repetitive micro-traumas of medical training can have a cumulative effect. It has been shown that trauma in general can limit a person’s sense of accomplishment, their relationship to happiness, and can impair their ability to form connections to others.
A study done in 2009 looked at both high and low points in the lives of interns. The high points described by interns typically included fostering connections, both with patients and with colleagues. It can be inferred then, if the ability and desire to connect with others is impaired due to micro-trauma, there is a danger of losing one of the only ‘high points’ during a particularly sensitive time in medical training.
Staying silent in what is quite clearly an epidemic is no longer an option. In a time when social media can play many roles, one of the most important may be reinforcing a feeling of connection. I recognize that I may be an anomaly in being able to find a family of support during my medical training, which was transformational in both my personal life and in my career. But there are many ways to form a bond. Reaching out to trainees and letting them know they’re not alone may be the difference between life and death. We all have a role to play.

Dr. Willett is an emergency physician in Northern California. You can find more of her writing on her website http://www.jessicakwillettmd.com.
Reach out and continue the conversation on twitter @jkwillettmd.