Mr. Philips, my elderly patient in Room 602, was looking better. He was eating more of his breakfast, smiling, even walking to the bathroom with little assistance. I was getting ready to call his daughter with the positive update when the nurse ran over to my computer station in a panic: "Philips just suddenly started vomiting blood. Blood pressure is dropping."
I would have to work quickly: get better IV access, transfuse blood, call the gastroenterologist, call the intensivist. I dreaded that this was happening on a weekend, when things move more slowly. First, I still needed to talk to his daughter. Her dad had been declining over the last year: memory issues, trouble swallowing, saying he felt at the end of his life. Thankfully she answered the phone and I explained the urgency of the current clinical situation. The gastroenterologist would likely recommend an endoscopy to locate the source of bleeding and intervene. But there were risks associated with the procedure, the anesthesia, the blood, and an ICU visit. And there was the optimistic chance the bleeding would self-resolve.
His daughter listened calmly and attentively. It always surprises me when patients and families can do this in the face of such terrible news. When she finally spoke, she asked the question I dread the most: "What are the chances this procedure will work?" In all honesty, I had no idea. Was my answer supposed to be based on my clinical experience (limited) or the literature (if it even existed)? I could explain the risks and the benefits, but I could not help her weigh those chances. The truth is, I had never seen how a patient with his specific comorbidities was doing months after a procedure like this. "Let me call the specialists and get back to you," I mumbled, praying they would have a better, more detailed answer. And yet, even with their years of clinical experience, their answer remained short and direct: "If we don't do this procedure, he could die."
During medical school and residency, I often saw a patient for an hour or so in the hospital or at an outpatient office, and then never again. Other times, I participated in the care of a patient for days straight, learning the intimate details of their life and body: their most involved family members, their favorite meals from the hospital cafeteria, how much they urinated each hour. But then the patient was discharged, or died, or more likely, I switched to a different medical service. Would Mrs. Gibson get insurance approval for her hepatitis medication? Would Mr. Simon survive his rare sinus cancer? Would Mrs. Lambert clear the bloodstream infection? I would never know. Since the end of residency, I have worked as a hospitalist, which is also purely shift-based work. I continue to have these fragmented clinical stories, unable to get to the final chapters of the illness narratives I see.
I often wonder how my past patients, the true teachers of medicine, are doing. This pattern of almost never reexamining the same patient has been the hardest challenge of my education and practice. How do I know if I truly made the right clinical decision if I am never told the outcome? Can I appropriately counsel a patient on expectations if all I have are unresolved clinical experiences? And would having this knowledge even benefit patients and families in complicated and nuanced decision-making, where there are so many uncontrolled variables impacting the outcome?
When there is a patient I become particularly fond of, or feel stumped by their medical presentation, I try to remember their name to later search the EMR system. I learned that Mr. Parks died from liver cancer two months after we discharged him from the hospital to follow up with oncology to begin treatment. I wondered how his wife was grieving. I learned that Mr. Kelly eventually saw a neurologist after three months of waiting and was diagnosed with Parkinson’s disease. I wondered if his symptoms had improved. I saw that Mrs. Knight decided to get the imaging of her brain and chest, and it did in fact show metastatic lung cancer. I wondered who told her the news and what treatment, if any, she would choose. And Mr. Phillips? He did have the endoscopy, and the source of bleeding was cauterized. He developed significant delirium, possibly related to the anesthesia and a prolonged hospitalization, and was ultimately discharged to his nursing facility on hospice.
What I wish existed is an automated system in the EMR to set up alerts of patients previously cared for. I feel this would be especially beneficial for us shift-based practitioners, including residents, hospitalists, intensivists, inpatient consultants, and EM doctors. Yes, there are the ethics around the privacy of EMR that need to be considered, as well as the risk of overwhelming providers with alerts and additional medical information. But the benefit is that we would be able to counsel future patients more effectively based on more comprehensive past clinical experience. Another thought is to incorporate this kind of long-term thinking into medical training. Perhaps we should be required in medical school or residency to go back and visit (or at the very least, read about) the patients we helped previously care for.
So often in our lives we act on instincts. We hope for the best, we plan for the worst. But with decisions that affect health and well-being, I want people to be able to make the most informed choices. I worry that with the current model of medical education, I constantly fall short of providing comprehensive information to my patients when guiding medical decision-making. For now, I will try to provide full care and treatment while only knowing half the story of my previous patients. And I will keep trying to look for any opportunity to learn about these final chapters of my patients.
How do you follow your patients' stories? Share in the comments how you balance care continuity and shift-work.
Charlotte Grinberg is an oncology hospitalist at Beth Israel Hospital in Boston, MA. She has a particular interest in palliative care and narrative writing. Her writing has appeared in JAMA, Health Affairs, and the Annals of Internal Medicine. She is a 2020–2021 Doximity Op-Med Fellow. All names and identifying information have been modified to protect patient privacy.
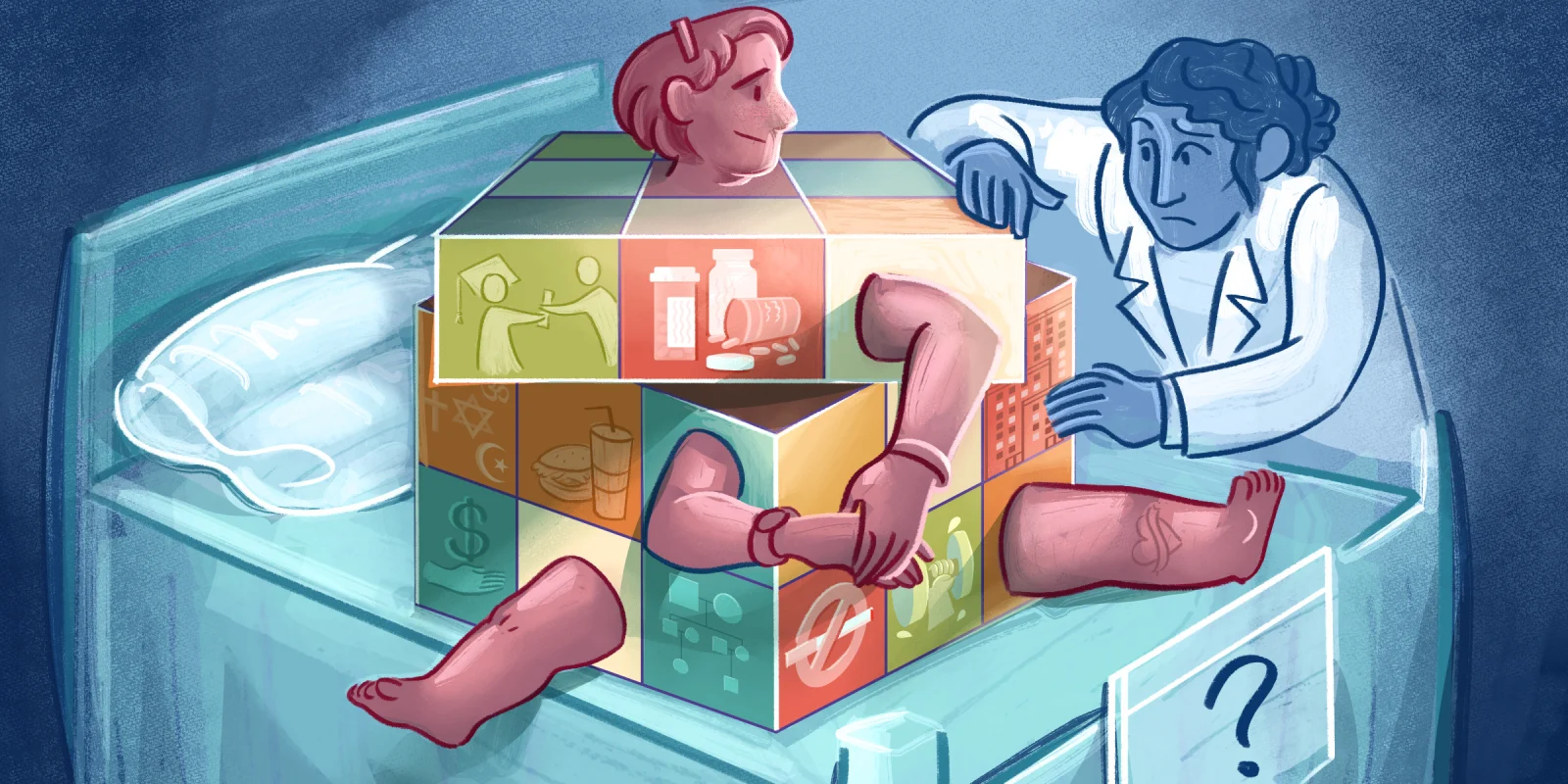
Illustration by April Brust