I quietly knock on the door and enter. The sunlight streaming in belies the heavy stillness in Ms. M’s room. My eyes settle on a poster assembled by her family with photos recounting rosier times, nearly all of which show her sporting a big smile. I shake myself out of this trance, running through my routinized pre-rounds checklist in my head — “How did the night go? Any pain or discomfort?" — yet, this time seems different. Twenty-four hours ago, we had huddled around her bed as we shared the devastating news that her cancer had spread to her brain, there were no further disease-targeted therapies available, and that we feared her time might be short — days to weeks. It was the first time she and her family had engaged in such a discussion of prognosis. As I nudge her out of her fitful slumber, she greets me warmly, her once radiant smile contorted into a grimace from the pain of the suppurating mass growing outwardly from her chest wall and infiltrating her lungs, a near-constant reminder of the disease that leaves her life teetering on the precipice. “I’m scared, Doc,” she whispers. My breath catches. As I peer into her eyes, I see my own mortality. Nobody at her young age should have to hastily arrange their affairs; she frets about the mounting medical bills and who will care for her children. I have few words to comfort her, so I sit, head bowed, holding her hand until my pager wrests me from this solemnity.
Such scenes, as I have come to realize as an internal medicine resident, are all too commonplace in the setting of metastatic cancer. There is a morbid joke that abounds — “Why do coffins have nails in them? To stop oncologists from administering another round of chemotherapy.” As I have witnessed firsthand, oncologists care deeply about their patients, and yet, simultaneously, there appears to be an either unintentional or willful under-appreciation of the necessity of discussing prognosis early and often with patients, particularly those with stage IV cancer. As in Ms. M’s case, it became apparent that, in the several years that she had battled cancer, few of her doctors had broached the incurable nature of her disease. The writing was on the wall — she had relapsed with every chemotherapy regimen. And yet, in her time of need, when the cancer had invaded her brain, bereaving her of the ability to move her legs, her oncologist balked at visiting Ms. M to convey the implications of this development, leaving it instead to her primary inpatient medicine team to do so. This baffled me. As a young, first-year resident at the time, it seemed spineless.
As I have reflected on why this occurred, I have come to a few conclusions. First, the “C” word (cancer) remains a bogeyman within the public’s collective consciousness. Nearly 1-in-2 Americans still believe that “most of the time, cancer is a rapidly terminal disease.” Cancer, quite literally, represents an ontological threat for patients — their body in revolt, its insidiousness a manifestation of the intricate machinery of homeostasis gone awry. Having broken the news of a new cancer diagnosis to many individuals, I have come to recognize the achingly emotional nature of these discussions. Oncologists see their charge as offering hope (glossed as prolonging life) and may fear that admitting that a patient might die from his/her cancer might make it a fait accompli. Previous work has suggested that truthful discussions about prognosis, even when dire, do not rob patients of hope, begging the question of whether we are doing more harm by avoiding such discussions.
Second, the advent of immunotherapy and small-molecule inhibitors has led to a shift from “therapeutic nihilism” to “therapeutic optimism.” Whether the surfeit of new, difficult-to-pronounce drugs has actually changed overall survival is debatable, the attendant prognostic uncertainty is not. As my colleagues and I have previously reported, this prognostic uncertainty is prevalent and affects if prognostic discussions happen and when they happen. Third, most cancer care occurs in the clinic. Most significant cancer complications, from intractable vomiting to febrile neutropenia to malignant bowel obstructions, are cared for in the hospital. Oncologists often see their patients when times are good; as a resident, I see the underbelly of cancer on the inpatient side. This time-space discontinuity also means that the pressure of discussing prognosis in the clinic diminishes; symptoms at bay, talk can easily turn to the logistical aspects of the next round of chemoradiation.
And yet, the deferral of prognostic discussions unsurprisingly yields quite discrepant understandings between patients and their oncologists in terms of the severity of the cancer and the intent of therapy. Several studies, however, have reported that cancer patients desire more prognostic information. The discordance between oncologists’ and patients’ understanding of prognosis can have dire consequences particularly with respect to decisions regarding life-sustaining care. My colleagues and I often feel exasperated when individuals with widely metastatic cancer elect to be full code when it’s dubious whether such measures will meaningfully change prognosis. At least in some circumstances, the request to “do everything” is a plaintive wish for more time as the mask of prognostic ignorance is unceremoniously removed. In Ms. M’s case, immediate and extended family assembled at her bedside offering succor while her life-force waned. I wonder how they would have spent that time had it been made clear to them earlier that her cancer’s inexorable march could not be quelled.
The charge to care for someone with a life-limiting condition is a sacred one. As others have averred, with cancer, we can “hope for the best” but must “prepare for the worst.” Patients often take our lead, sometimes out of fear or out of false reassurance, when we do not ask them regarding their desire to know their prognosis. As Don Berwick has mused, “we are not priests in a cathedral of technology.” The ethical obligation of physicians vis-à-vis their patients can be embodied as a commitment to non-abandonment, particularly when the limits of medicine are reached. Such a stance reminds us to remain humble in the face of the myriad ways in which the human body can fail us and cues us to remember the most basic acts of caregiving, including the laying of hands and attending to the emotions that accompany those nearing the end of life. At the same time, recognizing the challenges in having prognostic discussions, we all ought to take a page from the playbook of our palliative care colleagues who have offered us several avenues to approach these difficult conversations and with the added peace-of-mind that early palliative care involvement may actually contribute to both improved quantity and quality of life. We ought not be purveyors of false hope lest our patients stare back, Janus-faced, asking, “Why have you forsaken me?”
How do you approach conversations about prognosis with your cancer patients? Share in the comments.
Dr. Anand Habib is a third-year internal medicine resident at University of California, San Francisco. Originally from Houston, Dr. Habib completed his undergraduate work with honors at Stanford, worked as a Global Health Fellow at a clinic in Haiti's central plateau, finished a masters degree with distinction in Medical Anthropology at Oxford University as a Rhodes Scholar, and earned a medical degree from Harvard Medical School. He has previously studied the use of therapies for hematologic malignancies and oncologists' feelings of prognostic uncertainty in advanced lung cancer and is currently pursuing interests at the nexus of ethics, health policy, and distributive justice. He is a 2021–2022 Doximity Op-Med Fellow.
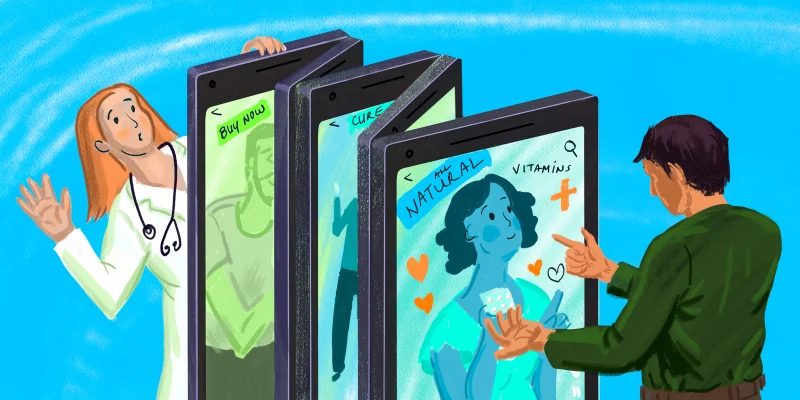
Illustration by April Brust