“I want fried chicken and collard greens please,” she said, her dark brown eyes looking straight into my soul. She was a less than 5-foot-tall wizened older woman sitting in her wheelchair with a blue blanket (her favorite color) on her legs. She had her hands crossed and was smiling up at me expectantly. Ms. G felt she was living in a hotel and this was a pleasant delusion for her, so the staff and I did not try to reorient her. She was close to 100 years old, and I paused to consider this request. I could get fried chicken from a local fast food place, but where would I get collard greens? I have always felt that at 100 years old you should have what you want to eat as much as possible.
I knew how to make collard greens, but my cooking left much to be desired. It was good I went to school to be a psychiatric NP and not a chef! I decided I would think about it more at home and see if I could bring her some next week. I told her so and did a little dance to cheer her up. She pronounced it was "awful" and her roommate laughed and laughed. As I left, she said to her roommate, “The staff at this hotel are just not very accommodating sometimes.”
I went from her room to go see the man that the residents referred to as, “a tall drink of water.” He was around 6 feet, 6 inches tall when he stood with his walker, and rail-thin with gray tousled hair on his head that always reminded me of Albert Einstein. Mr. W was lying in bed with the covers up to his neck and was drowsy as his pain medications for terminal cancer were kicking in. When I walked in and touched his shoulder, he looked up at me with his pale blue eyes and smiled broadly. He started telling me about his latest naughty audiobook which was blaring in the background on his too-loud headphones.
He was mostly deaf and had a former roommate who was a preacher (who had also been a patient of mine). The preacher complained about “the loud dirty sinful books” that Mr. W listened to “all of the time!” I sat down and listened and indeed the audiobook playing was a torrid romance that made me blush. Mr. W loved them though, so he was given the headphones, which did not help much since they were turned up so high. His current roommate was totally deaf and did not mind a bit.
He took quite a long time telling me about the book’s doomed romance. I felt as if his description, while entertaining, was taking a lot of time and I needed to hurry up and go see my other patients, so I told him I had other patients to visit, and that I would be back next week and went on my way.
I did not know that the next week I would be sitting in my home office looking at the online charts, as so many of my patients died there of COVID-19, both Ms. G and Mr. W included. If I had known, I would have run out and at least gotten Ms. G fried chicken, and listened longer to Mr. W describing that saucy story.
I sat helplessly because I was not allowed into the nursing home, as COVID-19 did what the pandemic of 1919, the Great Depression, war, pneumonia, and numerous other trials and tribulations had not been able to do to my geriatric patients. It was fast and so deadly that most died within three days.
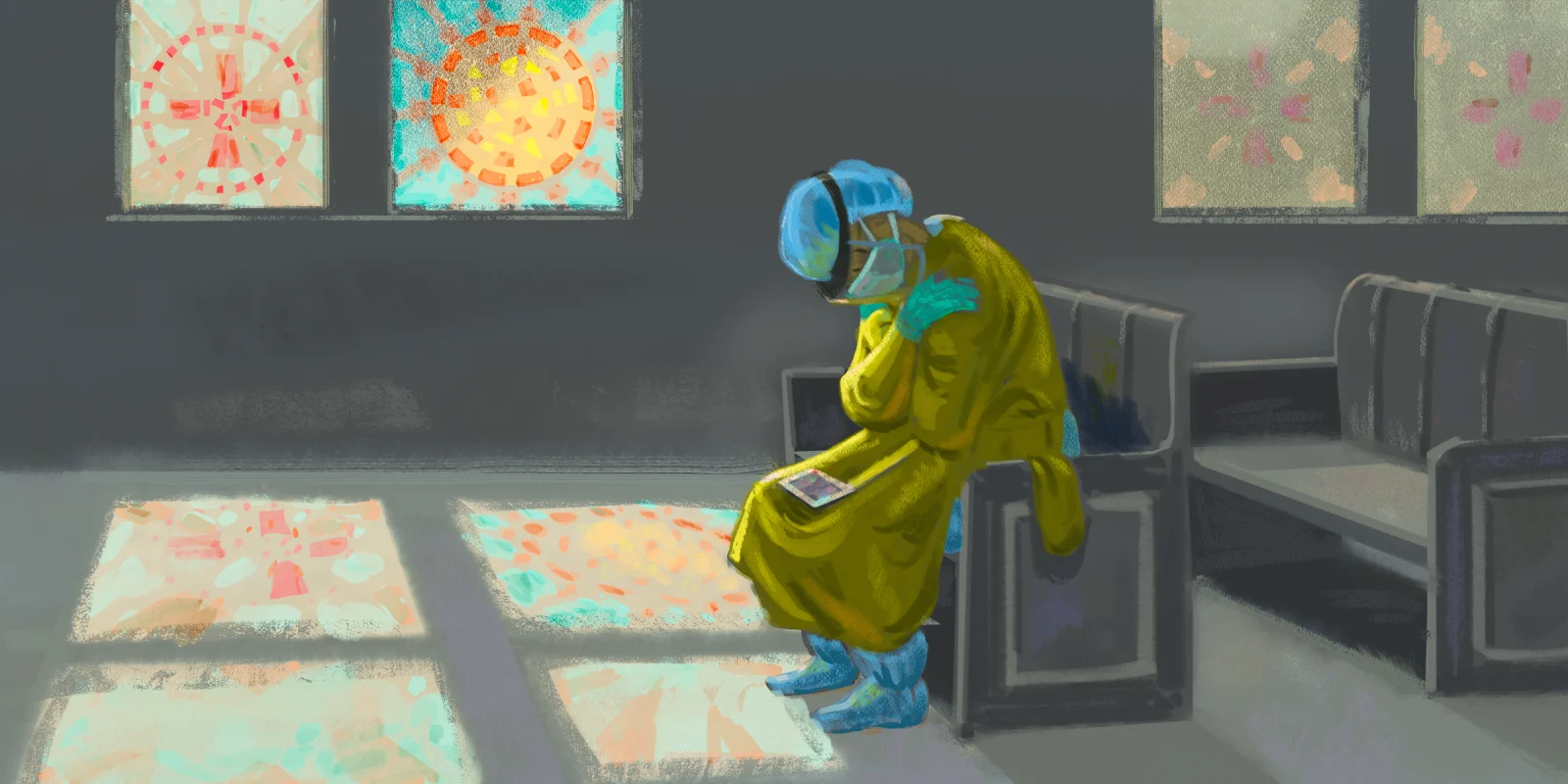
Weeks later, I was allowed back into the facility in full COVID-19 isolation gear. The empty rooms and sad looks on the staff’s faces were heartwrenching. People say, “hindsight is 20/20,” but that doesn’t make it hurt any less.
I found a site for health care workers who needed to talk to someone and I spoke with an Episcopalian priest via Zoom. She said what health care workers were experiencing was “displaced grief.” We did not get to go to the funerals or memorials due to the coronavirus. Due to this, we had nowhere to go with our sadness. She suggested we talk about my favorite patients and I talked about Mr. W and his racy books. I laughed and cried and it felt wonderful to have a time and place to grieve.
So far, I have had around 120 of my patients die from COVID-19 at numerous nursing homes. It is a terrible killer loose in the geriatric community. I want to encourage my fellow health care workers to reach out to someone if they need help with their grieving. This much loss is almost unfathomable and I know my soul gets weary and my energy gets drained sometimes. I am sure that other health care workers are suffering this way as well. We love and care about people, that is why we do the jobs we do. But sometimes we need to take care of ourselves, too.
Laura Goodwin a psychiatric-mental health NP who has worked with the elderly for 15 years. She was the 2011 psychiatric provider of the year at her company, and does telemedicine as well as site-based visits at area nursing homes and assisted living facilities.
All names and identifying information have been modified to protect patient privacy.
Illustration by Jennifer Bogartz