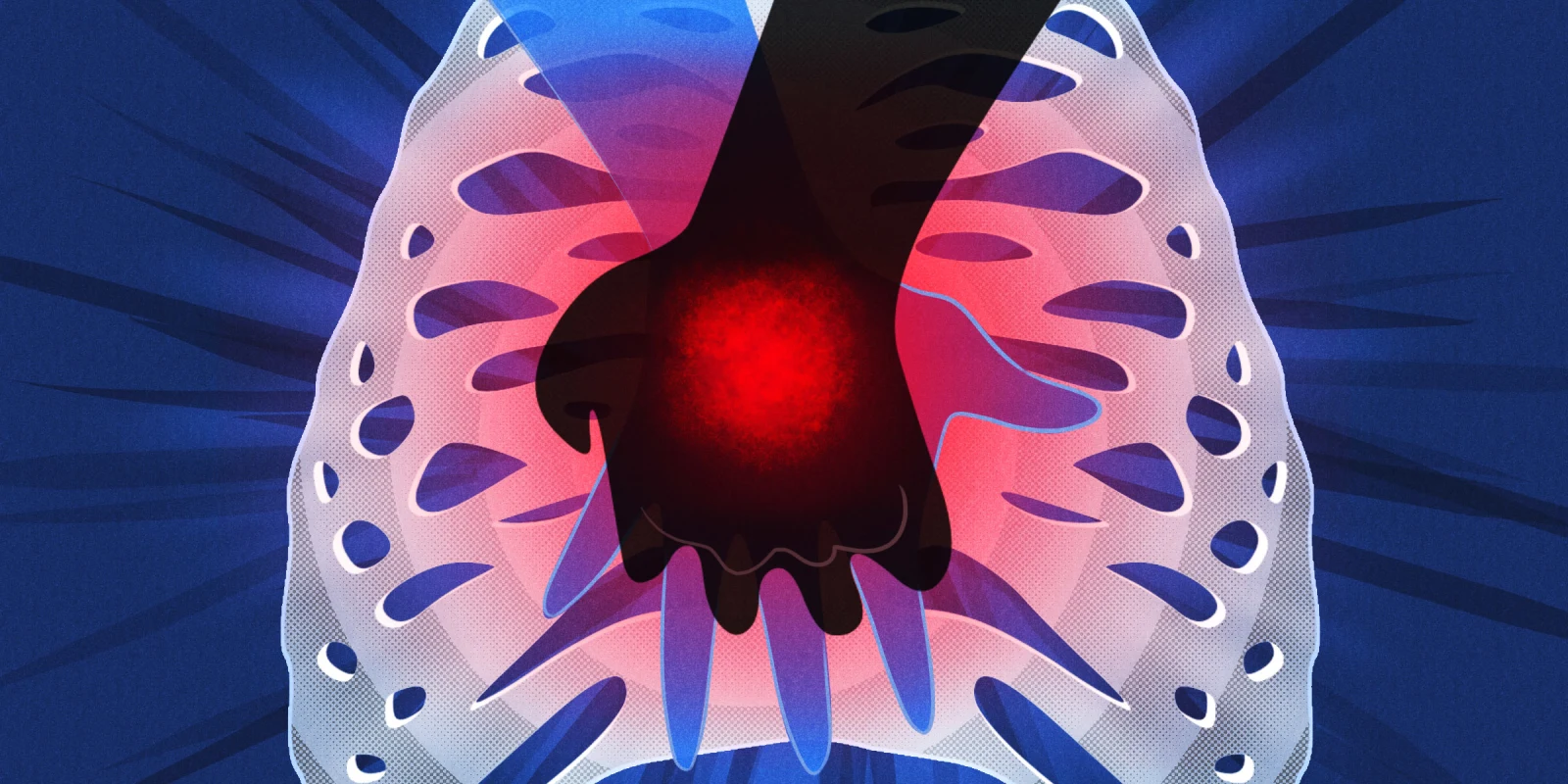
Illustration by April Brust
Illustration by April Brust
In the Hippocratic Oath, we swore to uphold the preeminent value so intrinsic to medicine: to do good. Yet, we often forget that perhaps of equal or greater value is "to do no harm." Of course, it's easier said than done. With advances in medicine, the balance of costs and benefits becomes ever so difficult to discern. As such, we elect to do absolutely all that we can, and provide treatments that may at times have little to no benefit and yet all the potential for harm. I’m referring to cardiopulmonary resuscitation (CPR).
Every day, patients “code” and receive CPR as a life-saving therapy. While some are brought back to life, however fleeting, many more die after sustaining aggressive resuscitation efforts; their lives hanging by a thread and their bodies adorned with lines, tubes, catheters, and riddled with evidence of iatrogenic trauma in the aftermath of heroism. Those who end up on ventilators for days to weeks or longer often suffer complications such as pneumonia, bleeding, stroke, and severe myopathies or neuropathies from which they may never recover. So it begs the question, why do so many patients undergo CPR even when it can cause so much pain and suffering?
In one instance while training in the intensive care unit, I had the opportunity to work closely with the palliative team that assisted us with a family meeting for goals-of-care discussion. The patient was their elderly father that presented with a major second stroke and superimposed aspiration pneumonia. He was functionally dependent and had heart failure, cirrhosis, end-stage renal disease on dialysis, and a history of major stroke. In spite of optimal medical therapy, his clinical course deteriorated and we could see that death was imminent.
Naturally, "code status" was a distinct component of our discussion. Despite the notable imbalance of harm over benefit for CPR in this patient, he was kept “full code” because family members perceived “DNR/DNI” to mean "giving up," a common misconception held even by some doctors. I remember the discomfort and struggle we experienced as we tried unsuccessfully to reconcile the family's perception of DNR/DNI with ours. In fact, a large number of physicians experience uneasiness discussing end-of-life care and recommending DNR/DNI where it may be appropriate. In the end, we performed CPR when the patient suffered cardiac arrest, and miraculously, we brought him back to life after over 45 minutes of chest compressions. However, he remained in critical condition in a coma, on a ventilator and four vasopressors, and with no signs of recovery.
Why did we practice CPR? Not because we recommended it, but because we were afraid to refuse it. As physicians, we often feel obligated to offer CPR regardless of the clinical picture. Only after the family saw the aftermath of the prolonged resuscitation efforts did they come to understand that CPR is not the end-all-be-all of medicine. From that point on, they elected for compassionate extubation, to let him die in peace with the utmost comfort he deserved. However, he has already suffered because we could not refuse to do CPR.
In a culture where doctors understand the harms of CPR, it is still offered in excess. Some believe that it is the only chance the patient has to survive, and not offering it is the same as killing the patient. However, CPR is a procedure like any other, and surgeons certainly know when to refuse surgery when the risk is prohibitively high, whatever slim life-saving potential may exist. There is a time for CPR and one for DNR/DNI. As the advocates for our patients, we should recommend what is appropriate, and remember "to do no harm."
In the Hippocratic Oath, we swore to uphold the preeminent value so intrinsic to medicine: to do good. Yet, we often forget that perhaps of equal or greater value is "to do no harm." Of course, it's easier said than done. With advances in medicine, the balance of costs and benefits becomes ever so difficult to discern. As such, we elect to do absolutely all that we can, and provide treatments that may at times have little to no benefit and yet all the potential for harm. I’m referring to cardiopulmonary resuscitation (CPR).
Peter Z. Xu is a first year cardiology fellow at LAC USC Medical Center and has no conflicts of interest.