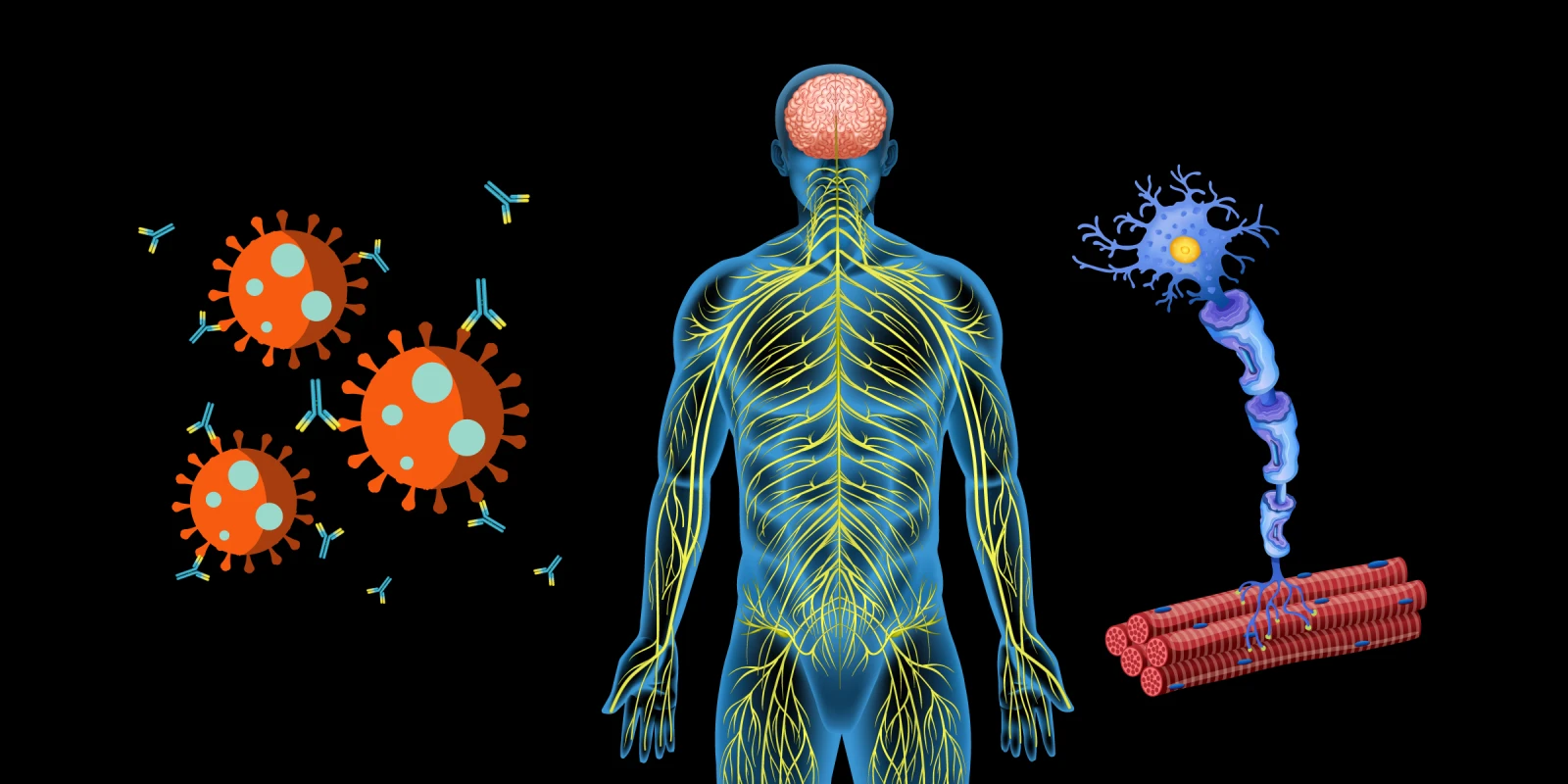
SARS-CoV-2 is a novel coronavirus causing the ongoing COVID-19 pandemic. Early studies showed that morbidity/mortality from this highly infectious virus is largely driven by a strong inflammatory response causing acute respiratory distress syndrome. Little information was initially available about the impact of SARS-CoV-2 on persons with a compromised immune system, including patients with chronic diseases such as MS on immune therapies. Indeed, the risk of COVID infection and vaccine efficacy are frequent concerns raised by patients.
Small early studies suggested that MS patients on disease-modifying therapies (DMTs) had a similar risk of morbidity/mortality as the general population. A previous Austrian study of 126 patients with MS who were diagnosed with COVID-19 infection found that 86.5% had a mild course, 9.5% a severe course, and 3.2% died from COVID-19. After adjusting for comorbidities, this study found that exposure to MS DMTs, including immunosuppressive DMTs, was not associated with COVID-19 severity or mortality.
Recent larger registry data have suggested differing risk patterns. The MS Data Alliance COVID-19 study of 5,543 patients with suspected (17%) or confirmed (83%) COVID-19 infection looked at associations with DMTs and COVID-19 severity. The authors found that male sex, older age, progressive MS, and higher disability were associated with worse outcomes from SARS-CoV-2 infection. In contrast to the smaller studies, when compared to other DMTs, ocrelizumab and rituximab were associated with higher frequencies of hospitalizations, [aOR=1.61(95%CI=1.06-2.43); aOR=2.42(95%CI=1.54-3.81)] and ICU admission, [aOR=3.13(95%CI=1.22-8.00); aOR=4.46(95%CI=1.64-12.09)]. Rituximab was associated with increased risk of artificial ventilation [(aOR=3.57(95%CI=1.38-9.20)] with a non-significant, positive trend for ocrelizumab [aOR=1.86(95%CI=0.76-4.55)]. Lastly, rituximab was associated with higher frequencies of death.
Interim analysis from 1339 patients treated at 35 Italian MS centers participating in the CovaXiMS study in Italy compared SARS-CoV-2 antibody levels before and after mRNA vaccination. Patients receiving fingolimod, rituximab or ocrelizumab had lower SARS-CoV-2 antibody titers after their second vaccine dose than patients receiving other DMTs, including natalizumab and cladribine, with higher antibody titers induced by the Moderna vaccine. However, unlike antibody responses, SARS-CoV-2 memory T-cell response to vaccination was robust for patients receiving ocrelizumab but not fingolimod. Similarly, T-cell responses were robust for patients on other DMTs, including cladribine. Based upon updated data, guidelines regarding vaccination and DMTs in MS patients are expected.
As the DMT landscape continues to evolve, balancing vaccine efficacy and infection risk continues to be vital. Data presented at the 2021 European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS) meeting regarding COVID-19 infections and vaccine efficacy provide much-needed information to MS patients and clinicians as they navigate through this pandemic. Until additional guidance is available, it remains incumbent upon treating physicians to have detailed discussions about current evidence with patients.
Dr. Lincoln is employed by McGovern Medical School and UT Health. He has received grants from EMD-Serono, the Department of Defense, and the National Institutes of Health, has received participation fees from Sanofi-Genzyme, and lecturing fees from Biogen and Bristol Myers Squibb.
Image by blueringmedia / GettyImages