As the cancer management evolves into precision medicine faster than ever before, international cancer meetings continue to bring novel approaches to our practice. Although the ASCO Gastrointestinal Cancers Symposium (ASCO GI) 2020 has not brought practice-changing data to our daily base practice life, it did provide further insight into the evolution of management of gastrointestinal cancers.
The management of locally advanced resectable gastroesophageal junction (GEJ) adenocarcinoma has been in debate since the release of the FLOT4 trial data (Al-Batran et al Lancet 2019), which showed improvement in overall survival outcomes as compared to perioperative ECF/ECX. Although there is no clinical data to compare this regimen with the current of the standard of care carboplatin/paclitaxel based chemoradiation (CRT), clinical practice has already substantially shifted away from CRT. At this time, the most rational approach of treating GEJ patients who have high-risk of systemic recurrence (N2 disease) would be FLOT, whereas GEJ patients with high-risk of local recurrence (large local disease) should be considered for CRT. Interim PET CT for response evaluation (PET-adapted therapy) could guide clinicians for continuation vs. change of the approach (FLOT vs. CRT) and likely be the standard care of practice of the future. Mismatch repair (MMR) status evaluation may provide essential clues for the choice of treatment approach as the growing data suggest that patients with MMR deficiency may not benefit from systemic chemotherapy as good as MMR proficient patients do, suggesting CRT as a reasonable choice in these patients based on rectal cancer data in MMR-deficient rectal cancer patients.
The growing evidence from ASCO GI 2020 patients with systemic disease should be considered upfront molecular profiling with NGS-based technology to identify molecular targets such as HER2, MMR deficiency, and PD-L1 status. Progression of disease can be assessed by performing liquid biopsy-based ctDNA to better understand the mechanism of resistance as well as the dominant clone driving the disease in the setting of tumor heterogeneity.
Hepatocellular carcinoma (HCC) had significant evolution in the recent decade with the change of the second-line therapy and most recently IMbrave 150 trial led to the change of the first line of therapy after decades and Atezolizumab in combination bevacizumab replacing the role of sorafenib. The ASCO GI 2020 data further suggested that the combination of immune checkpoint inhibitor (ICIs) with tyrosine kinase inhibitors (TKIs) will likely be the future of HCC management (Yau et al ASCO GI 2020). On the other side, pancreatic adenocarcinoma (PDAC) remains one of the most challenging cancer and with continuing disappointing results in stroma targeting approaches. HALO-3 trial, phase III study of PEGPH20 which depletes tumor stroma, showed no improvement in survival outcomes when added to gemcitabine and Abraxane. SEQUELA trial investigated the efficacy of stroma modifying effect of IL-10 to optimize tumor microenvironment for anticancer immunity in PDAC and this study also failed to reach its endpoints. Altogether these data suggest that we have to redefine the role tumor stroma in the management of PDAC. The answer doesn’t appear to be as simple as depleting dense stroma. DNA damage response (DDR) defective (BRCA and PALB2 mutated) PDAC is seen in a minority subset of PDAC patients and recent progress led to practice change with the use of PARP inhibitor (Olaparib) in the maintenance setting (POLO-3 trial). ASCO GI 2020 data clearly showed the addition of PAPR to platinum-based chemotherapy is not a viable choice in this subset of PDAC patients (O’Reilly et al ASCO GI 2020). However, Cisplatin appears to be a more potent platinum agent and led to promising outcomes in BRCA and PALB2 mutated PDAC patients (O’Reilly et al ASCO GI 2020).
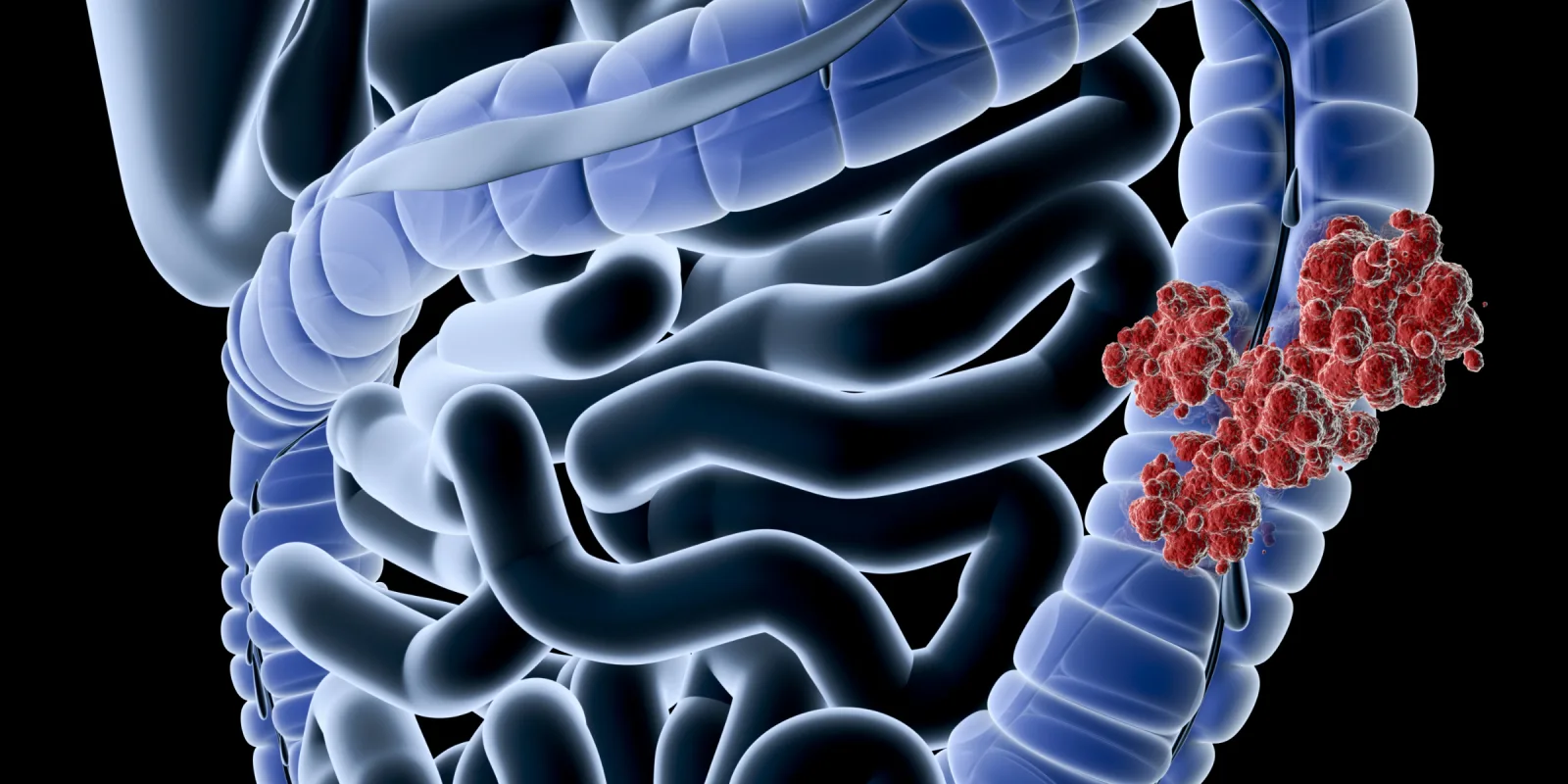
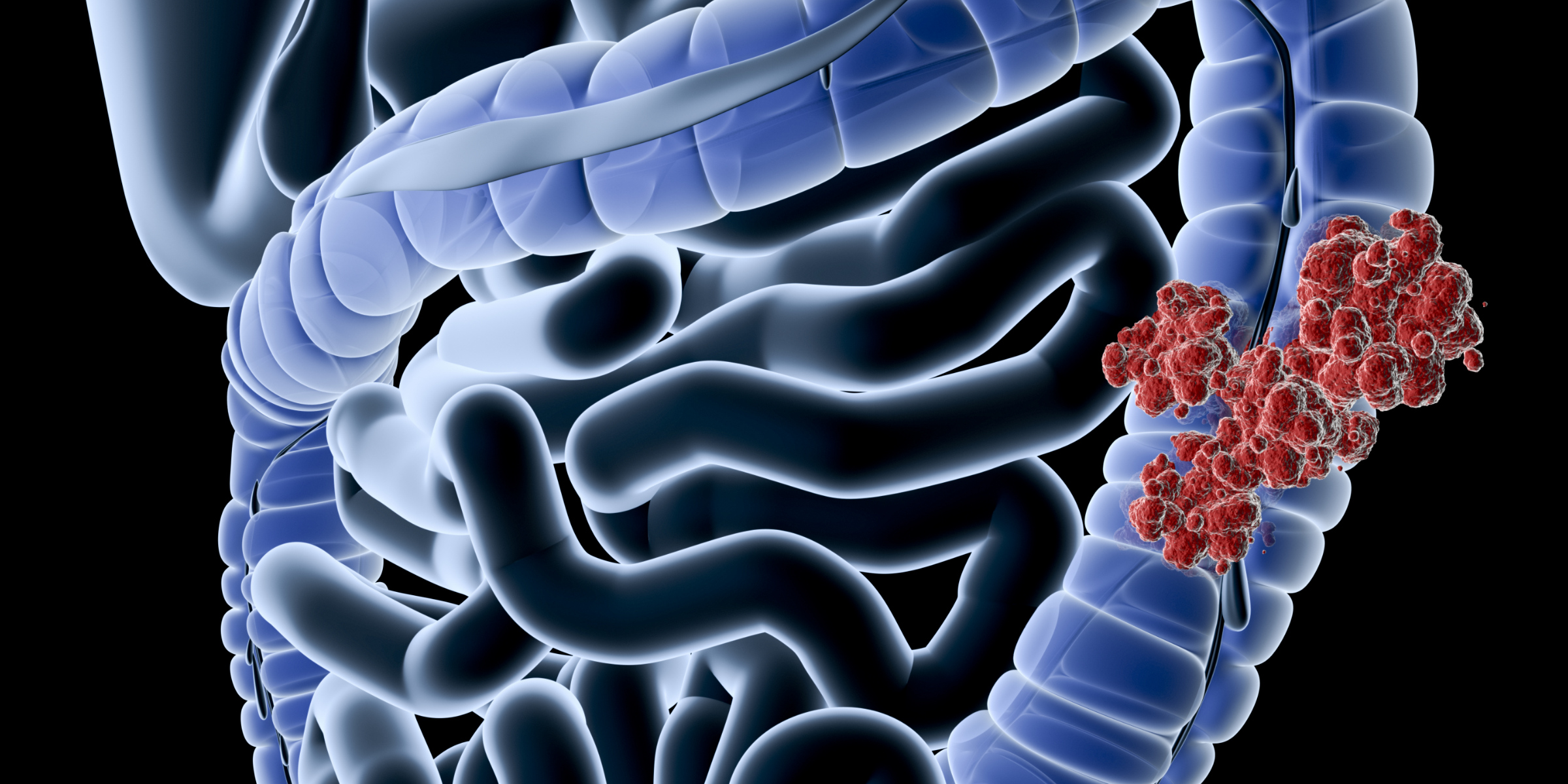
Colorectal cancer (CRC) is one of the gastrointestinal cancers that achieved substantial improvement in therapeutic options. BEACON trial and other BRAF-targeting approaches opened the BRAF box for targeting therapy and the future holds promise for this field. Novel combination approaches will likely continue to evolve in the near future in BRAF mutant CRC. Similar head-spinning changes have been developing in MMR-deficient CRC and ICI therapy will likely move to first-line therapy in the near future for this subset of CRC patients (Lenz et al ASCO GI 2020). The BRAF-mutant subset of MMR deficient CRC may behave differently with the early progression of disease when treated with ICIs (Sahin et al ASCO GI 2020). The progress also continues to evolve for adjuvant therapy of colon cancer patients, with the future holding likely implementation of risk-adapted adjuvant therapy with the use of biomarkers such as CD3+ CD8+ T cells (immunoscore) and ctDNA (Pages et al ASCO GI 2020, Morris et al ASCO GI 2020).
Overall, The ASCO GI 2020 projected a future practice of gastrointestinal oncology with more personalized approaches and risk-adapted systemic therapies in patients who underwent upfront definitive therapy. As science continues to evolve, these novel approaches will likely continue to improve the quality and length of life of our patients.