Dr. Joshua Davis is a 2020–2021 Doximity Research Review Fellow. Nothing in this article is intended nor implied to constitute professional medical advice or endorsement. The views expressed in this article are those of the author and do not necessarily reflect the views/position of Doximity.
Are COVID-19 Patients Really Hypercoagulable?
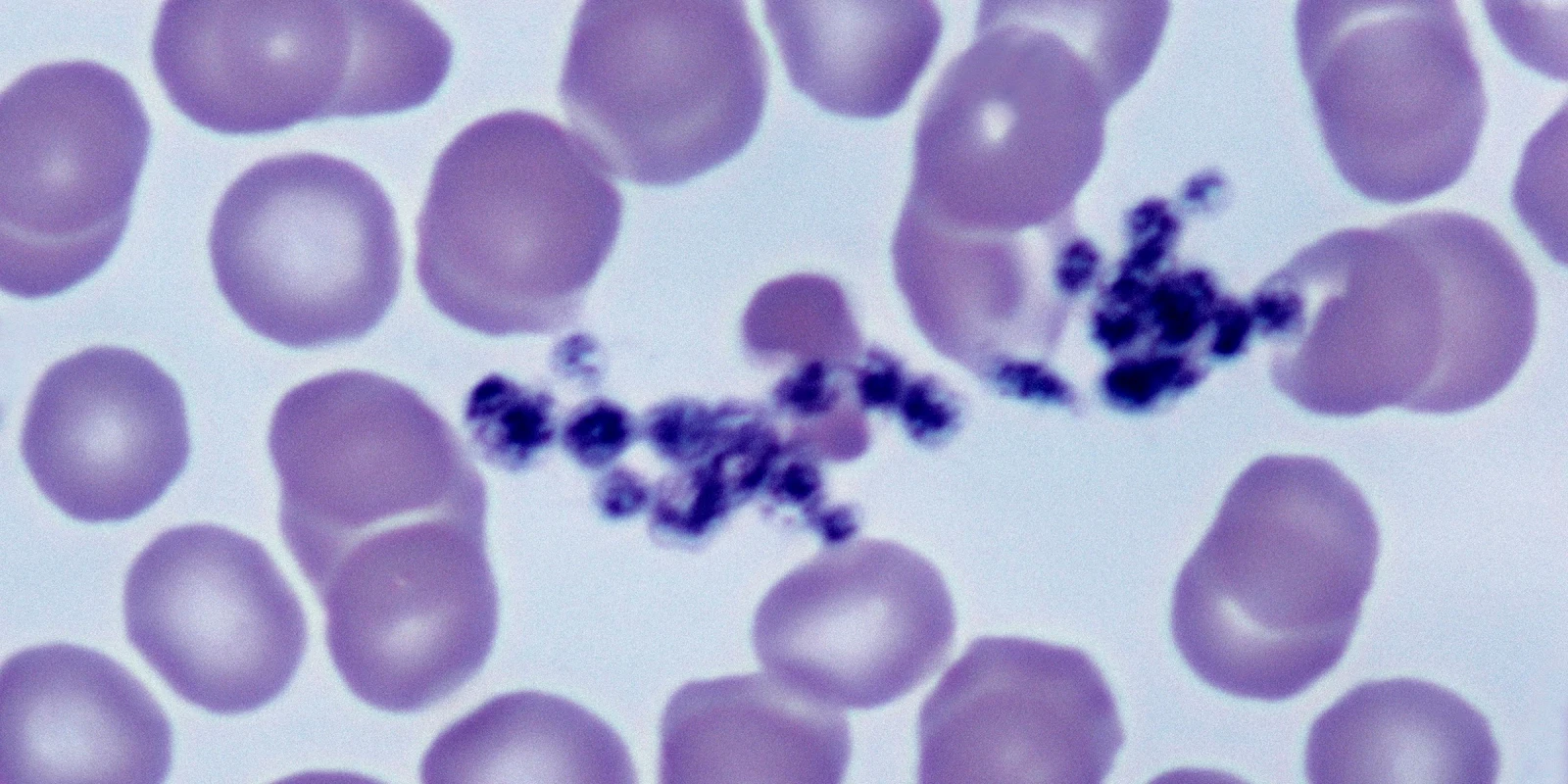
Many clinicians suspect that SARS-CoV-2 infection produces a hypercoagulable state. There is some in vitro data that COVID-19 alters platelet function and autopsy data shows a large number of VTE in these patients. There have also been reports of frequent thromboembolic events among critically ill patients, including rapid clotting of central venous, dialysis, and arterial catheters. A markedly elevated D-dimer is relatively common in hospitalized patients and is known to be a poor prognostic indicator. Observational studies have shown that hospitalized patients who receive anticoagulation have lower mortality than those who do not. Many hospitals have implemented full therapeutic dose anticoagulation for high-risk admitted patients, even without documentation of a venous or arterial thrombus. Some ER physicians are even recommending a short course of full-dose (325 mg) aspirin to discharged patients with COVID-19. But all of this evidence is observational and speculative; whether COVID-19 is, in fact, associated with an increased risk of clotting is still in question.
To evaluate the relationship between COVID-19 and hypercoagulability further, researchers conducted an international retrospective study of all patients having a CT pulmonary angiogram. Their data suggested that there is not an increased risk of pulmonary embolism in patients with COVID-19.
Notwithstanding this recent study, some hospitals have already developed protocols for anticoagulating inpatients based on D-dimer results. Most of them use levels well above the laboratory cutoff value. This leaves the emergency physician in a conundrum: should the physician order a D-dimer in the ED, knowing that it may lead to an unnecessary CT or an unnecessary delay to admission?
Currently, whether we should anticoagulate or prescribe aspirin to outpatients with an elevated D-dimer also remains unresolved. There is no data to support the practice, and patients safe for discharge from the ER likely do not need anticoagulation. There are some hospitals discharging high-risk admitted patients on prolonged anticoagulation. Outside of orthopedic surgery, aspirin has a limited role in preventing VTE and really is only helpful in arterial clotting. In some prior comparisons, risks are similar between full anticoagulation and aspirin, despite the belief that aspirin is safer.
As a practicing EM physician, what will I be doing regarding coagulopathy in the COVID-19 context? I will continue to use D-dimer as a diagnostic screening test for VTE in low-risk patients. Historically, I have had a lower threshold to consider testing COVID-19 patients for VTE, but this study makes me question my practice. I will probably stop testing COVID-19 patients that are PERC negative with a D-dimer. I do not routinely order a D-dimer as a prognostic indicator and will continue to not do so. The inpatient care team can determine the need for a D-dimer test and act on any positive results. I also do not prescribe aspirin or anticoagulation to outpatients and will continue to not do so.
Dr. Joshua Davis is an emergency physician who completed his residency at Penn State Milton S. Hershey Medical Center. He completed medical school at Thomas Jefferson University and received his undergraduate degree from the University of Delaware. His research interests are broad and include emergency medicine topics along with patient safety, handoff communication, and diet and exercise.
Click here to see more perspectives on COVID-19 from the Doximity network.
Click here for up-to-date news about COVID-19 on Doximity.